For those of you who struggle with SIBO, IBS, and other gastrointestinal disorders, I have some very good news! Recent research into a natural approach to relief shows that about three out of four people with IBS had their symptoms ease right away after starting a low-FODMAP diet. They felt the most relief after seven days or more on the plan. As a physician dedicated to empowering you to take back your health, I rarely get to use the words “right away” in discussing a solution, so I am excited to share this with you.
The research showing that diet plays a huge role in gastrointestinal pain relief is a pretty big deal. 15% of the world’s population, or one in seven people, are affected by IBS.1 Following testing, as many 50% of those people are found to have SIBO, or Small Intestine Bacterial Overgrowth.2 We’re talking about millions and millions of people who can take control of their health problems by changing their diet.
Who Can Benefit from a Low-FODMAP Diet?
People Dealing with IBS or SIBO
The topic is not well understood by conventional medicine and practitioners, so let’s clarify what IBS and SIBO really are.
Irritable bowel syndrome (IBS) is a diagnosis of exclusion. When someone has stomach pain, gas, bloating, and irregular bowel movements without physical damage to the gastrointestinal system, and they don’t show signs of another disorder, conventional medicine will label the issue IBS.
SIBO is an overgrowth of bacteria in the small intestine. The bacteria normally found in the colon and large intestine spread to the small intestine where it should not be found. It can also be bacteria typically found in the small intestine that has grown unchecked.3 Signs that you may have SIBO include IBS symptoms as well as vitamin deficiencies, skin rashes, and other systemic problems that you might not associate with gastrointestinal issues. This quiz can help you find out if SIBO is really to blame for your IBS.
Patients Struggling with Histamine Intolerance
SIBO could be behind the sudden development of histamine intolerance because SIBO can lead to an increase in food sensitivities. Histamines are the chemicals that tell your body to create inflammation. SIBO can trigger an inflammatory response for a variety of reasons, so SIBO and histamine intolerance often go hand-in-hand. The symptoms can be localized in the stomach and appear as cramps or found throughout the body. Symptoms include unexplained rashes, flushing, fatigue, swelling, headaches, hypertension, pain, and bloating among others. As you’ll see, avoiding high-FODMAP foods can drastically reduce histamine release.
What is a Low-FODMAP Diet?
Now that we know more about SIBO and IBS, let’s find out how a low-FODMAP diet can help. Researchers at Monash University in Melbourne, Australia developed a popular diet plan limiting certain kinds of carbohydrates that can irritate the digestive system. This is a tool to help relieve distressing and painful symptoms while you work toward treating the root cause. It is not a diet plan to help you lose weight. The intention is to limit, for a short period, short-chain carbohydrates (sugars). These carbs are fermentable oligo-, di-, and monosaccharides, and polyols. Researchers simplified these terms into the acronym FODMAP. Here’s what each of these five words means:
- Fermentable: This refers to the process in which gut bacteria ferment undigested carbs producing gases.
- Oligosaccharides: These are sugars including fructans and galacto-oligosaccharides (GOS) found in wheat, barley, onions, garlic and legumes.
- Disaccharides: Think lactose, which is found in dairy products such as milk, soft cheeses, and yogurt.
- Monosaccharides: Fructose, a simple sugar found in honey, apples, high fructose corn syrup, and agave.
- Polyols: These include sorbitol and mannitol, which are found in some fruit and vegetables and are used in artificial sweeteners.
These carbohydrates are absorbed very slowly or they are completely indigestible. They can draw water away from the rest of the body into the bowel and cause imbalances. Gut bacteria trying to break down these carbs ferment them, producing gas. While restricting high-FODMAP food doesn’t appear to affect bowel activity, it does impact the release of histamines that cause your immune system to go into overdrive.4 Fewer histamines released means less inflammation and irritation.
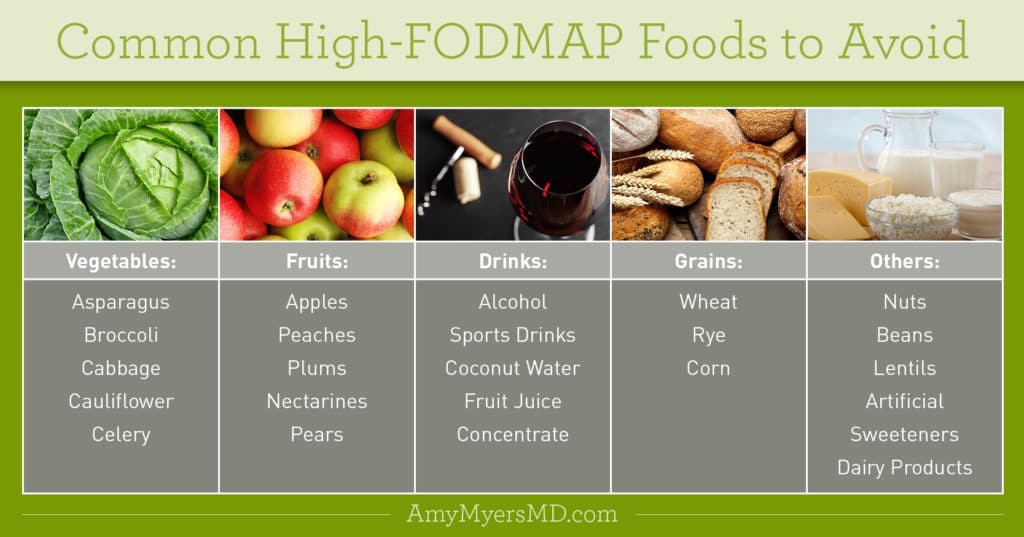
Researchers at Monash University produced a comprehensive list of high- and low-FODMAP foods and they continue to evaluate additional choices. Here is a chart of some of the more common high-FODMAP foods to avoid:5
 Dr. Amy Myers
January 28th, 2019
https://content.amymyersmd.com/article/low-fodmap-diet/Common High FODMAP Foods To Avoid – Infographic – Amy Myers MD®
Dr. Amy Myers
January 28th, 2019
https://content.amymyersmd.com/article/low-fodmap-diet/Common High FODMAP Foods To Avoid – Infographic – Amy Myers MD®FOODS to Enjoy on a Low-FODMAP Diet
Aside from relief from uncomfortable symptoms, one of the best parts about this eating plan is that it’s rich in all types of protein including fish, poultry, beef, lamb, and pork, as well as FODMAP vegetables including spinach and zucchini. Protein powders can also be a valuable part of a low-FODMAP diet, however, be careful to check the ingredients. You’ll want to avoid any that include whey, dairy or pea proteins. If you do opt for a protein powder for a breakfast smoothie or snack, I recommend my Paleo Protein powder, which is sourced from non-GMO, hormone and antibiotic-free, grass-fed beef.
Do you think a Low-FODMAP diet is right for you? Take this short symptoms quiz to determine which foods are best for your condition, and those you should eliminate from your diet.
Foods to Enjoy, Foods to Toss Quiz
How to Follow a Low-FODMAP Diet
The plan calls for a three-step approach. In step one, you’ll restrict your intake of high-FODMAP foods to reduce distress. Once your symptoms have resolved, you’ll move on to steps two and three. In step two, you’ll reintroduce foods one at a time into your diet, and monitor your reactions to determine which ones you can tolerate, and which ones cause problems. The final step is learning to balance high-FODMAP foods with low-FODMAP choices in terms of quantity and frequency.
Step 1: The Low FODMAP Phase
For two to six weeks, you toss all toxic and irritating foods and eat only low-FODMAP foods. During this period, enjoy meals featuring satisfying, high-quality proteins such as organic chicken and beef, vegetables such as zucchini, bok choy, and carrots, as well as fruits such as pineapple, cantaloupe, and grapes. It’s critical that you strictly avoid high-FODMAP foods to stave off a potential immune response.
Step 2: The Reintroduction Phase
Here, over a period of eight to 12 weeks, you reintroduce foods one at a time, a small amount at a time, and assess how you feel after each reintroduction. If something doesn’t feel right, eliminate that food and don’t add anything new for a few days.
If you feel fine, try increasing the amount of the introduced food, or increasing the frequency you eat it. Keep notes and focus on how each new food makes you feel. It is empowering to check in with your body about and respond to its needs.
Step 3: The Balance Phase
This is where you learn to find a balance among foods that don’t bother you at all, foods that you can eat sparingly, and foods that you should avoid completely. For example, you may find you can eat only half an apple if you are eating other high-FODMAP foods, but you can enjoy a whole one if you are eating only low-FODMAP foods otherwise.6 This will be completely unique to you, as though you’re creating your own FODMAP food list.
Treating the Root Cause to Beat Your Symptoms for Good
Easing your symptoms will provide physical relief and increase your confidence in taking control of your health. However, the long-term solution is identifying and treating the underlying cause of your sensitivity to high-FODMAP foods. In most cases, this means addresses SIBO.
To help you do that, I created a comprehensive 30-day program. This program includes a dietary protocol specially designed to address SIBO, FODMAPs, and histamines. It also includes targeted supplements to prune back the overgrown bacteria, reseed your large intestine with good bacteria, and provide detox support as the overgrown bacteria die off.
The SIBO Breakthrough® Program contains the complete set of tools you need to overcome SIBO. It includes meal plans, recipes, shopping guides, and pharmaceutical-grade supplements. That’s in addition to receiving all the support you need to regain control of your health and find success!
Article Sources
- https://www.monashfodmap.com/.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4250883/.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2890937/.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5390324/.
- https://www.medicinenet.com/low_fodmap_diet_list_of_foods_to_eat_and_avoid/article.htm#what_is_a_fodmap_elimination_diet.
- https://www.monashfodmap.com/ibs-central/i-have-ibs/starting-the-low-fodmap-diet/.
