Multiple sclerosis (MS) is a progressive autoimmune disease that affects more than 2.8 million people worldwide. The early phase of MS is called clinically isolated syndrome, which is the first onset of neurological symptoms that last for at least 24 hours.1
Clinically isolated syndrome (CIS) can be difficult to diagnose for several reasons. For one, symptoms of CIS can be vague and nonspecific. Additionally, some people with clinically isolated syndrome may not have visible lesions on an MRI scan, which is one of the primary signs of multiple sclerosis. I’ll talk more about that later.
Conventional medicine will tell you that nothing can be done to treat multiple sclerosis or stop it from progressing. You will be given harsh medications that suppress the immune system and manage your symptoms. As a functional medicine doctor and autoimmune patient, I know there is a better way!
Functional medicine takes a different approach to multiple sclerosis. You can reverse your condition and eliminate your symptoms by getting to the root cause. I will tell you about my proven approach to reversing autoimmunity that I’ve used on thousands of patients and seen amazing results. Before I get into that, let’s talk more about multiple sclerosis and clinically isolated syndrome.
What is Clinically Isolated Syndrome (CIS)?
Clinically isolated syndrome (CIS) is the first phase of multiple sclerosis, an autoimmune disease where your immune system attacks the myelin that protects your nerves. The inflammation, or demyelination in your central nervous system, causes neurological symptoms. In people with CIS, these symptoms last at least 24 hours.
CIS can occur at any age, yet it most often affects people between the ages of 20 and 40 and is more common in women than men. People with clinically isolated syndrome may or may not develop multiple sclerosis. However, a diagnosis of CIS can be an important indication of an increased risk of developing MS.2
Diagnosis of Clinically Isolated Syndrome
Clinically isolated syndrome can be challenging to diagnose. For one, the symptoms of CIS can be vague and nonspecific. They can also vary depending on which part of your central nervous system is being attacked by your immune system.
Visible lesions in the central nervous system during a magnetic resonance imaging (MRI) scan indicate CIS.3 However, some people with CIS may not have any visible lesions on a scan, which can make it harder to identify the underlying cause of their symptoms, which I will discuss shortly.
CIS is typically diagnosed based on a combination of a person’s medical history, symptoms, and results of neurological tests. Additional tests, such as cerebrospinal fluid (CSF) analysis, can also confirm a diagnosis.
In some cases, doctors may also perform a visual evoked potential (VEP) test to evaluate the function of the optic nerve, which can be affected by multiple sclerosis.
Symptoms of Clinically Isolated Syndrome:
As I mentioned, symptoms of CIS vary widely depending on the part of the affected central nervous system. Common symptoms of clinically isolated syndrome include:4
- Vision problems, such as blurred vision, double vision, or loss of vision in one eye
- Numbness or tingling in the face, arms, legs, or torso
- Muscle weakness or stiffness
- Problems with coordination or balance, such as difficulty walking or standing
- Problems with speech or swallowing
- Fatigue
- Dizziness
If you are experiencing these symptoms, talk with your functional medicine doctor about multiple sclerosis so you can begin to address the root cause of your symptoms and stop the progression into the later phases of multiple sclerosis.
Prognosis of Clinically Isolated Syndrome
The prognosis of clinically isolated syndrome depends on a number of factors, such as the severity and duration of symptoms, the extent of damage to the nervous system, and your age and health.
Some people with clinically isolated syndrome may never develop MS, while others may experience further neurological symptoms within a few years. The risk of developing MS after a diagnosis of CIS is estimated to be between 60% and 80%.
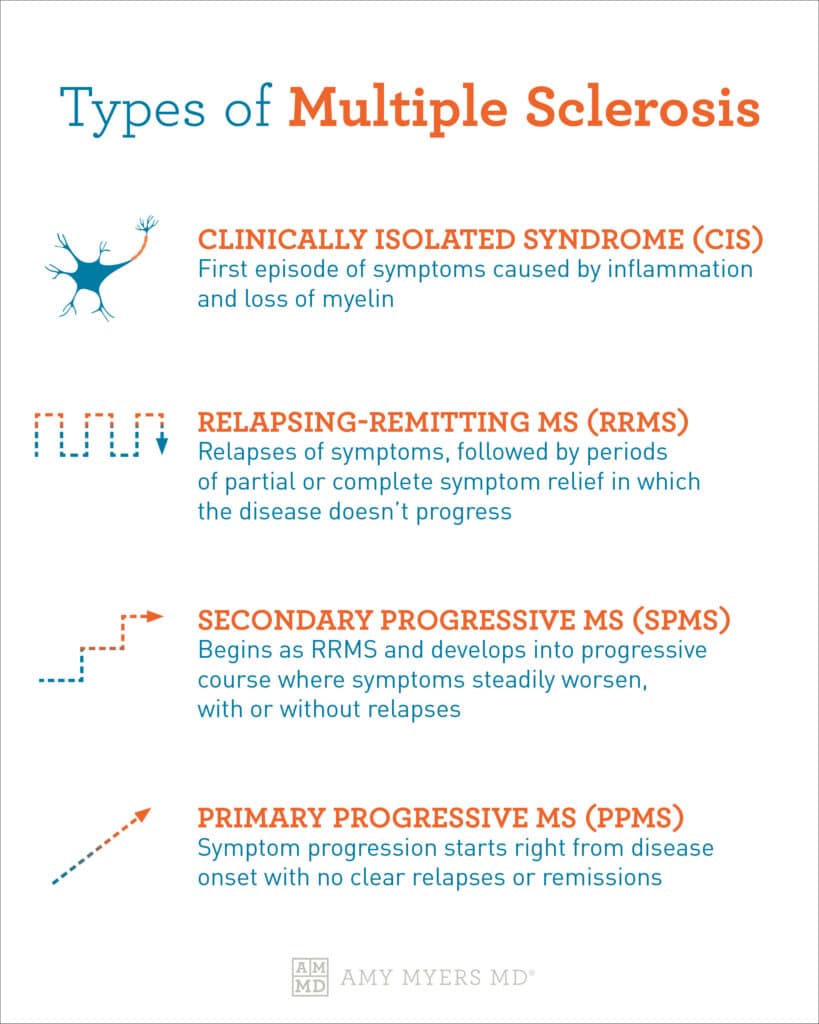
Multiple sclerosis is a progressive autoimmune disease, and clinically isolated syndrome is the first course of multiple sclerosis. Let’s get more into the types of multiple sclerosis.
Types of Multiple Sclerosis
Once multiple sclerosis progresses out of CIS, it enters relapsing-remitting MS (RRMS), then primary progressive MS (PPMS), and secondary progressive MS (SPMS). RRMS is the most common type of MS, affecting 85% of people diagnosed with multiple sclerosis. The good news is that you can change the course and reverse your condition regardless of how far along you are on the autoimmune spectrum. I’ll tell you more about my proven solution in just a bit.
I’ve told you about clinically isolated syndrome and how it’s the first stage of multiple sclerosis. Although CIS is the term used to define an isolated episode, there is a risk it will advance.
 Dr. Amy Myers
February 28th, 2023
https://content.amymyersmd.com/article/clinically-isolated-syndrome/clinically isolated syndrome – infographic – Amy Myers MD®
Dr. Amy Myers
February 28th, 2023
https://content.amymyersmd.com/article/clinically-isolated-syndrome/clinically isolated syndrome – infographic – Amy Myers MD®Relapsing-Remitting MS (RRMS)
RRMS is the most common type of multiple sclerosis, and when MS gets diagnosed. Diagnoses are most common among people in their 20s and 30s. However, you can get diagnosed later in life.
RRMS happens when new attacks (relapses or exacerbations) cause new symptoms, followed by partial or complete symptom relief periods. Common symptoms of RRMS include fatigue, vision problems, bowel and bladder problems, numbness, and neurological problems such as brain fog.
Secondary Progressive MS (SPMS)
SPMS follows the relapsing-remitting course of MS. Though not as common as RRMS, some people will progress into SPMS, where nerve function worsens. This is typically when most people with MS become disabled.
Secondary progressive multiple sclerosis is characterized by either active (with relapses) or inactive, as well as with or without progression.
Primary Progressive MS (PPMS)
Primary progressive MS (PPMS) is the final course of multiple sclerosis. A steady decline in neurologic function from diagnosis characterizes it, and there are no exacerbations and no remission period.5
The number of those diagnosed with MS that progress to PPMS is about 10%, and symptoms usually start between the ages of 35 and 39. PPMS usually causes more spinal cord than brain lesions, leading to difficulty walking.
What Causes Multiple Sclerosis
Autoimmune disease is a disease of your immune system. It results from an immune system that has gone rogue and begun attacking healthy tissue. In the case of MS, your immune system attacks the protective coating around your nerves. So to figure out what is causing multiple sclerosis, we have to start with what caused the immune system to misfire in the first place. Here are five underlying causes of autoimmune disease.
- Leaky Gut – When you have a leaky gut, undigested food particles, microbes, and toxins get through your gut lining and into your bloodstream. Your immune system views these particles as foreign invaders and begins to attack them. This continual strain on your immune system eventually causes it to go haywire and end up attacking your own tissues by mistake.
- Gluten – Gluten is the number one culprit of leaky gut because it triggers the release of zonulin in your intestines, a chemical that tells your gut lining to “open up.” It is also highly inflammatory, meaning it can cause stress to your immune system.
- Exposure to toxins – A heavy toxic burden puts you at greater risk of developing an autoimmune disease.
- Infections – Scientists have long suspected that infections from bacteria, viruses, and other toxins were likely to blame as causes of autoimmune disease. There are now several infections, including Epstein-Barr (the virus that causes mono), Herpes Simplex 1 and 2, E. coli, linked to autoimmune diseases.
- Stress – When you have constant stressors, your immune system never really gets to turn off. Your inflammatory immune response is activated for too long and eventually goes rogue, attacking your bodily tissues. Pretty soon, your stress hormones try to suppress the response but go overboard, leaving you with a weakened immune system.
If you address the root cause of your autoimmunity, you can work your way down the autoimmune spectrum and reverse your condition! Let me tell you about my proven solution that I’ve used with thousands of patients and seen amazing results. I call it, The Myers Way®.
You Can Reverse Multiple Sclerosis
The conventional medicine approach to autoimmune disease, including multiple sclerosis, is one of specialization. You see a neurologist who treats the symptoms and the symptomatic organ if you have multiple sclerosis. In the case of multiple sclerosis, the nervous system with medications that suppress the immune system. This type of treatment is fundamentally flawed.
As a functional medicine doctor, and an autoimmune patient, I know there is a better way. One of the biggest myths of conventional medicine is that autoimmune disease can’t be reversed. You can reverse multiple sclerosis by getting to the root cause and supporting the immune system.
The Myers Way® is based on functional medicine, a medical approach rooted in science that looks at how all systems in the body interact with one another and seeks to get them functioning optimally. The Myers Way® aims to relieve and reverse your symptoms, helps you get off your harsh medication, and enables you to live a healthy, energetic, and pain-free life.
This approach rests on four pillars, each of which has been tested through extensive research and has seen amazing results with thousands of patients over my years of practice as a physician.
Pillar I: Heal Your Gut
You begin by healing the gut. In functional medicine, we use the proven 4R approach:
- Remove the bad – Get rid of things that negatively impact the environment of your GI tracts, such as toxins and inflammatory foods, as well as intestinal infections, such as SIBO and yeast overgrowth.
- Restore what’s missing — Add Gut Restore with Betaine and HCL and digestive enzymes to your daily regimen to help support digestion and nutrient absorption.
- Reinoculate with healthy bacteria — Restore beneficial bacteria with a probiotic supplement to re-establish a healthy balance of bacteria to heal your gut.
- Repair the gut — Provide the necessary nutrients to help the gut repair itself. Leaky Gut Revive® Max supports your immune system and gut lining. Adding collagen protein or drinking bone broth will also help to heal your gut.
Pillar II: Get Rid of Gluten, Grains, and Legumes
Once you’ve healed your gut, it’s time to make diet changes and eliminate foods such as gluten, grains, and legumes that cause damage to your intestinal tract and inflammation. I also recommend that those with autoimmune diseases avoid vegetables in the nightshade family, which includes peppers, tomatoes, and potatoes. These plants are very high in lectins that damage the gut lining, quickly enter the bloodstream, and do not break down in cooking.
Pillar III: Tame the Toxins
Many patients notice improvement after addressing the first two pillars. However, I knew more work was needed when I saw patients whose symptoms didn’t improve.
We are exposed to thousands of toxins daily in the water you drink, the air you breathe, food, cookware, cleaning products, and cosmetics.
Unfortunately, we cannot avoid toxins altogether. As such, the solution is to reduce your body’s toxic burden by:
- Buying clean skincare and body products
- Cleaning your air by getting a HEPA filter for your home. I use AIRDoctor® air filters in my home.
- Buy clean food and eat organic whenever possible. It can be expensive, so buy free-range chicken, grass-fed beef, and wild-caught seafood.
- Clean your water by installing water filters on your shower taps and sinks. I have a complete filtration system from Aquasana.
Pillar IV: Heal Your Infections and Relieve Your Stress
If your symptoms haven’t cleared up after addressing the first three pillars, it’s time to dig deeper. The fourth pillar of The Myers Way® focuses on healing your infections, such as herpes simples and Epstein-Barr, and relieving your stress.
To relieve stress, I suggest adopting daily stress-relieving strategies. A few of my favorites include breathing exercises, listening to music, dancing, taking a long walk, or practicing yoga.
The Final Word on Clinically Isolated Syndrome
Just because you have clinically isolated syndrome doesn’t mean you have to live with multiple sclerosis. Conventional medicine will tell you that CIS will likely progress into MS and that you will have to live with it for the rest of your life. I have seen the success of The Myers Way® personally, with my patients and myself. You have the power to take back your health!
Article Sources
- Clinically Isolated Syndrome (CIS). National Multiple Sclerosis Society. 2023.
- Clinically Isolated Syndromes: Clinical Characteristics, Differential Diagnosis, and Management. Husnu Efendi. Articles of Neuropsychiatry. 2015.
- Assessment of lesions on magnetic resonance imaging in multiple sclerosis: practical guidelines. Massimo Filippi, et al. Brain. 2019.
- Clinically Isolated Syndrome. Cedars Sinai. 2023.
- Relapsing-remitting MS (RRMS). National Multiple Sclerosis Society. 2023.
