Alzheimer’s disease can be a scary topic. Yet, here’s a truth you may not know: Unlike the rest of our bodies, our brains do not have to deteriorate as we age if we take care of them — and I’ll show you how. As my friend, the neurologist Dr. David Perlmutter, has said: “We are designed to be smart people our entire lives!”
With time, we may get wrinkles and need glasses. We may move more slowly, and our hair may turn grey. Contrary to popular belief, though, it is absolutely not true that we must lose our mental “sharpness” as the years pass.
That is a fallacy propagated by the prevalence of the degenerative brain diseases that affect 50 million people worldwide, with 10 million new cases each year. The most common of these diseases is Alzheimer’s disease.
The good news is that, like autoimmune disease,
Go Deeper
Discover where you fall on the autoimmune spectrum and how your gut health holds the key to reversing autoimmune diseases.
Alzheimer’s disease is primarily brought on by lifestyle. However, it does have a genetic component that I’ll address later. So it can be largely prevented by the right dietary and lifestyle choices. And I have even more good news: Alzheimer’s disease is the subject of much scientific study, and researchers are finding out that there is tremendous hope that we can turn the tide on this disease.
Let’s take a look at what exactly Alzheimer’s disease is and what you can do — starting today — to prevent or halt it!
What Is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia. It’s a degenerative brain disease with no known cure. However, new research is showing that we can influence its occurrence and progression. To better understand this disease, let’s take a look at how the brain functions.
Your brain is the complex “control center” of your body. Weighing only three pounds, it contains a massive network of 100 billion nerve cells (neurons), 100 trillion intersections of nerve cells (synapses), and 100 thousand miles of blood vessels.
Synapses transfer information through chemicals called neurotransmitters that are passed from one neuron to another in lightning-fast electrical bursts. Signals flow throughout this network of neurons and synapses, creating the foundation of thought, memory, emotions, and voluntary and involuntary movement.
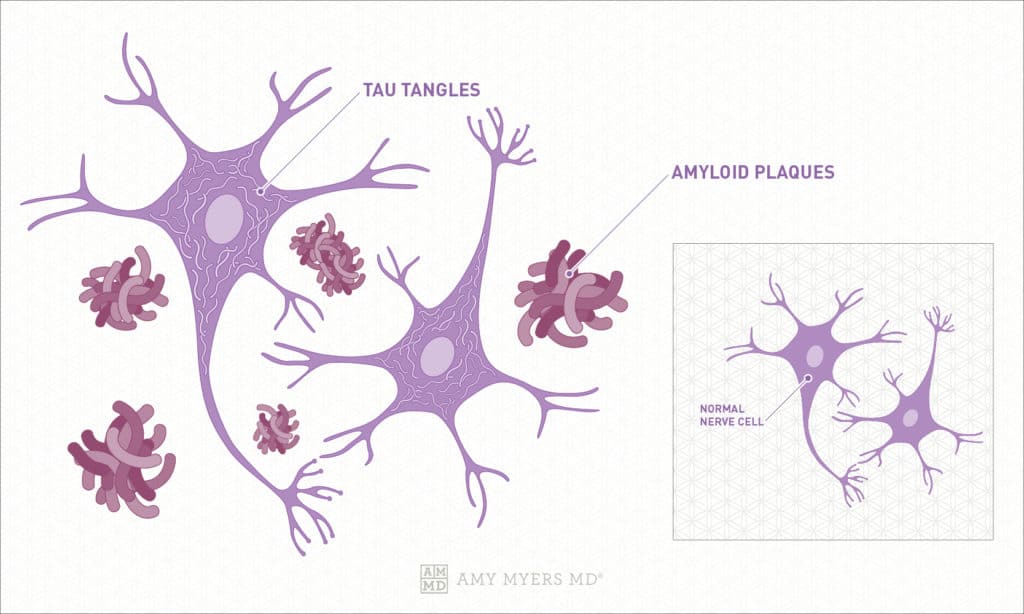
There are two proteins that are closely associated with Alzheimer’s disease. The first is the amyloid precursor protein. No one is sure of its exact function; however, scientists believe it may help neurons develop. This protein naturally breaks down into smaller parts that are cleared away in a healthy brain. One of these parts is a particularly sticky substance that forms beta-amyloid plaques.
In this disease, for reasons that are not yet understood, these plaques remain and even build up outside the neurons. This inhibits the transfer of signals at the brain’s synapses, impairing the transfer of information. These plaques tend to build up first in the part of the brain that deals with memory, although it is unclear why.
The second protein contributing to Alzheimer’s disease is a protein called tau, which forms “tau tangles” inside the brain’s neurons. These tangles disable the brain’s absorption of nutrients and other molecules in the neurons. Again, the process is not well understood.
 Dr. Amy Myers
October 25th, 2020
https://content.amymyersmd.com/article/halt-prevent-alzheimers-naturally/What Is Alzheimer’s? Tau Tangles, Amyloid Plaques – Infographics – Amy Myers MD®
Dr. Amy Myers
October 25th, 2020
https://content.amymyersmd.com/article/halt-prevent-alzheimers-naturally/What Is Alzheimer’s? Tau Tangles, Amyloid Plaques – Infographics – Amy Myers MD®We do know the damage to the brain’s neurons significantly impairs cognitive function related to learning and memory. As symptoms increase, an individual will show a decline in the ability to perform daily tasks, such as remembering to keep appointments. As Alzheimer’s disease continues to damage and destroy neurons, it impairs an individual’s ability to perform basic functions such as walking and even swallowing. In its final stages, it is fatal.
The Long-Term Development of Alzheimer’s Disease
Prevention is critical with this disease, as there is no cure. I know that sounds frightening, so let’s pause here, and I’ll return to the good news: At any point, you can slow or even stop Alzheimer’s disease with diet and lifestyle changes. Here’s why that’s possible — I’ll cover how to do it a bit later on.
The symptoms of Alzheimer’s disease can occur gradually over a period of up to 20 years. Recent studies have shown that those with genetic mutations that cause the disease have high levels of beta-amyloid in the brain as early as 22 years prior to diagnosis. Researchers also found that these individuals began to develop symptoms at the same age as their biological parent(s) with the disease, whether that was at the more typical age or as early-onset Alzheimer’s disease.
Another study showed the brain’s ability to metabolize glucose began to decrease 18 years prior to the diagnosis of Alzheimer’s disease, and brain atrophy appeared 13 years before the onset of Alzheimer’s. When an individual has early-onset Alzheimer’s, the brain mitigates its deficiencies. Yet, as time passes and neurons are further damaged, the brain can no longer compensate, and symptoms of the disease begin to surface. Beta-amyloid plaques and tau tangles also appear throughout the brain in areas other than cognition.
Diagnosis of Alzheimer’s used to depend on an examination of the brain after death, yet now we have cognitive tests and new imaging techniques that show plaques in the brain. I’ll cover those later in this article. Early detection is key, as there are three identified stages of Alzheimer’s. The stages of Alzheimer’s disease are the same for typical or early-onset Alzheimer’s disease.
The Three Stages of Alzheimer’s Disease
Let’s take a closer look at the three stages of Alzheimer’s to better understand this disease, which is now so prevalent. The stages of Alzheimer’s parallel the progression of the disease itself.
Stage One Alzheimer’s Disease: Preclinical
In the preclinical stage of Alzheimer’s disease, the brain has measurable changes in the cerebrospinal fluid and blood that show early signs. These are called biomarkers. At this stage of the disease, there are no perceivable symptoms, such as cognitive decline. While many people progress to the other stages of the disease, not every person who is at this stage of Alzheimer’s disease progresses to the next stage.
Stage Two Alzheimer’s Disease: Mild Cognitive Impairment (MCI)
In this stage of Alzheimer’s disease, people with mild cognitive impairment present with a biomarker of the disease (such as elevated beta-amyloid levels) and also have more cognitive decline than is typical for their age. These changes may not interfere severely with day-to-day activities yet may be apparent to family and friends. These early signs of Alzheimer’s disease include:
- Frequent memory loss (not just where the keys are located but what they are for)
- Confusion about locations and time
- Taking longer to accomplish normal daily tasks
- Trouble handling money and paying bills
- Loss of spontaneity and interest in enjoyable activities and hobbies
- Mood and personality changes such as depression
About 15 to 20 percent of people age 65 or older experience MCI, and these individuals are more likely to develop dementia from Alzheimer’s. Researchers have now labeled something called “subjective cognitive decline” in which older adults recognize a cognitive decline and the early signs of Alzheimer’s in themselves, and report it to their doctor for further evaluation.
Stage Three Alzheimer’s Disease: Dementia
This is the final stage of the disease. Dementia means that an individual’s productivity is impaired by cognitive decline in memory, thinking, and behavior. There is also evidence of Alzheimer’s disease in the brain, which can be tested and confirmed. The symptoms worsen over time at varying rates and progress from mild to moderate to severe.
In the mild stages of the disease, individuals are relatively independent, yet may require some monitoring for their own safety, as they can forget dates and locations. In the moderate stage — which is the longest — basic skills such as communicating and performing simple tasks decline. Mood and personality are also affected at this stage. Irritability, moodiness, and depression are common. At the severe stage of Alzheimer’s disease, 24-hour care is required, as individuals usually lose mobility. Their lack of movement makes them susceptible to life-threatening conditions such as lung infections and aspiration pneumonia because their muscles aren’t working to clear the body of excess fluids.
Who Is Affected By Alzheimer’s Disease?
The rate of Alzheimer’s disease is on the rise globally, and the statistics are a bit staggering. Let me outline what we know about who gets Alzheimer’s disease.
Over 5 million Americans have this disease, and it is the 6th leading cause of death in the United States. Two out of three people with this disease are women. Hispanic Americans and Black Americans are more likely to develop it than White Americans.
By 2050, it’s estimated there will be as many as 16 million Americans living with it. Every 66 seconds, someone in the United States develops Alzheimer’s disease, and one in three seniors dies with some form of dementia. In the US, Mississippi has a higher rate of Alzheimer’s disease mortality than any other state at 45.8%; New York is lowest at 13.1%.
As I mentioned before, 50 million people worldwide have Alzheimer’s or some form of dementia. Yet, only one in four people with this disease have been diagnosed. Alzheimer’s disease and dementia are most common in Western Europe with North America close behind. However, Alzheimer’s is least prevalent in Sub-Saharan Africa. There is a 68% projected increase in the global occurrence of dementia by 2050 in low and middle-income countries.
Do you remember I said that lifestyle played a big part in this disease? In fact, 30% of people with this disease also have heart disease, and 29% also have diabetes. In fact, Alzheimer’s disease is often referred to as Type 3 diabetes. An unhealthy heart cannot pump blood containing nutrients to the brain, thereby contributing to Alzheimer’s disease. Diabetes affects the body’s ability to process insulin, which delivers fuel to your brain.
What is Early-Onset Alzheimer’s Disease?
Early-onset Alzheimer’s is defined as of the disease in anyone younger than the age of 65. A total of 5% of those with Alzheimer’s disease get early-onset Alzheimer’s, or 200,000 people in the US alone. People with early-onset Alzheimer’s disease often have signs of apraxia, or impaired movement and speech due to brain damage. Those with early-onset Alzheimer’s also show visuospatial dysfunction. That is the loss of the sense of “whereness” in relation to yourself to your environment and in the relation of objects to each other.
Let’s take a look at genetic factors that contribute to both early-onset Alzheimer’s disease and the more typical form of the disease. I’ll also cover the tests that verify the presence of it.
Genetic Factors of Alzheimer’s Disease
Genetic factors account for 25% of autoimmune disease, and we have reason to suspect that Alzheimer’s disease may be related to autoimmunity. Genetics does play a role in the disease. Two categories of genes influence a person’s risk factor for developing Alzheimer’s disease: risk genes and deterministic genes.
Scientists have found Alzheimer’s genes in both categories. Less than 1% of Alzheimer’s cases are caused by deterministic genes (genes that cause disease, rather than increase the risk of developing a disease). One risk gene is the APOE-e4 gene. While everyone has an APOE gene, those with the -e4 allele are more likely to experience early-onset Alzheimer’s disease. Those who inherit one APOE-e4 allele have an increased chance of Alzheimer’s disease. Those who have two have an even greater chance. Approximately 40-65% of those with Alzheimer’s disease have this gene, which can be identified through a saliva test.
Tests for Alzheimer’s Disease
There are multiple methods of testing for Alzheimer’s disease. Many tests use something called a biomarker. This is a measurable biological factor that indicates the presence or absence of a disease, along with the risk of developing a disease or the progression of a disease. For example, a high blood glucose level is a biomarker of diabetes.
Doctors can check for biomarkers of this disease using positron emission tomography (PET) imaging. The amounts of beta-amyloid and abnormal tau in the brain can be seen on at PET scan. Doctors can also test for levels of these same proteins in cerebrospinal fluid and levels of particular groups of proteins in the blood.
A PET scan can also check levels of glucose metabolism in the brain using the radiotracer fluorodeoxyglucose. Finding a simple and inexpensive test, such as a blood test, to diagnose Alzheimer’s disease would be ideal for patients, physicians, and scientists. Research is underway to develop a low-cost blood test that can identify the disease up to 20 years before symptoms develop. It may be available as soon as 2023.
Finally, doctors can also conduct cognitive tests to measure mental acuity and can compare the results to a standard to establish the extent of brain damage. One common assessment is the Mini-Mental State Exam (MMSE), which measures a range of everyday mental skills. Another typical assessment is the Mini-Cog test which involves two tasks: remembering a list of objects and drawing the time on a clock. Both tests can be used with typical or early-onset Alzheimer’s disease.
Is Alzheimer’s Disease an Autoimmune Disease?
There is a strong correlation between autoimmunity and Alzheimer’s disease. That is more good news! If Alzheimer’s disease is indeed an autoimmune disorder — and we know how to address autoimmune disease — this can lead to better treatment options. Let’s explore the relationship.
The beta-amyloid plaques and tau proteins associated with Alzheimer’s disease are toxic, and this triggers the immune system cells in the brain called microglia. Microglia attempt to clear these harmful proteins as well as the dead and dying cells they normally clear up. Inflammation occurs when the microglia are unable to keep up with all the dead and damaged cells that need to be cleared.
As we know, chronic inflammation is the root cause of autoimmunity. As the inflammation may well have been going on for years before any symptoms of the disease are perceived, researchers suspect that the microglia get confused over time by the plaque buildup and begin to attack healthy brain cells in addition to simply clearing the brain of dead or dying cells. This immune system malfunction may be a culprit in the progression of Alzheimer’s disease, or even a cause of the disease itself.
Further evidence of the connection between Alzheimer’s disease and autoimmunity is that some recent studies have shown an improvement in cognitive tests of Alzheimer’s patients who received an anti-inflammatory drug. The drug, etanercept, is an autoimmune suppressant that conventional medicine uses to treat rheumatoid arthritis, RA. RA has a similar inflammatory response to Alzheimer’s disease.
What To Do To Prevent or Halt Alzheimer’s Disease
This is the empowering part! You can take back control of your health and prevent or stop Alzheimer’s disease by using my 4R approach to banishing the inflammation that can lead to autoimmune disease and Alzheimer’s. Even if you or a loved one do start to have symptoms, a change in habits can help slow the progression of this disease. Researchers have discovered a process called neurogenesis which is dictated by your DNA.
More specifically, a gene called BDNF, or brain-derived neurotrophic factor, supports the formation of neurons, protects existing neurons, and promotes synapse formation. The gene that controls BDNF is activated by lifestyle habits including exercise, caloric restriction, a ketogenic diet, and nutrients such as curcumin and the Omega-3 fat DHA.
Whether or not you are worried about preventing or halting Alzheimer’s disease, a diet rich in anti-inflammatory foods is a good idea. Along with exercise, mental activities, meditation, and good sleep, you can change the trajectory of your brain health now and later in life. Let’s take a closer look at how you can implement brain-boosting habits.
Change Your Diet
There are foods you’ll want to avoid, as well as ones you’ll want to emphasize in your diet to decrease your chances of Alzheimer’s disease. Limit the number of carbohydrates in your diet. Avoid:
- Inflammatory foods including:
- Gluten
- Dairy
- Grains
- Pseudograins
- Nightshades
- Eggs
- Toxic foods such as:
- Alcohol
- GMOs
- Sugar
- Packaged and highly processed foods
- Focus instead on:
- Berries
- Coconut or MCT oil
- Curcumin
- Garlic
- Green tea
- Proteins including wild-caught fatty fish, grass-fed meats, and organic chicken
- Saffron
- Olive oil
- Onion
- Vegetables, especially dark, leafy greens
Intermittent fasting and reducing your caloric intake by 30% has also been shown to improve cognitive function. Caloric restriction simply means eating 30% less food than you would on a normal basis.
A ketogenic diet is ideal for the brain, as it is high in fat, which is the nutrient your brain needs most. I discuss the basics of the ketogenic diet in this article. Discuss these diet options with your healthcare professional before making any changes. This is particularly important for those of you with autoimmunity who struggle to keep weight on.
Exercise Your Mind
To have lifelong brain health, it is imperative to develop new neural pathways in your brain. You can do this by giving your brain a good “workout.” The best way to do this is to challenge your mental acuity by studying something complex that requires keen mental focus. Keep it interesting and fun!
Go Deeper
Take control of your brain health by implementing these 7 Ways to Improve Memory and Focus.
Learn a new language or pick up a new activity such as basic coding, baking, or woodworking. The more interested you are in the subject and the more rewarding the activity, the greater the impact on your brain. Other ways to exercise your brain include:
- Puzzles and other games
- Memorization of poetry or song lyrics
- Playing an instrument
- Meditation (yes, learning to relax your mind helps brain health!)
Get Enough Sleep
While you sleep your brain flushes out toxins such as beta-amyloid which contributes to Alzheimer’s disease. As you age, you tend to spend less time in the deep stages of sleep where fact-based memories as well as emotional and procedural memories are made.
Go Deeper
Having trouble sleeping? Get to the bottom of the problem so that you can start sleeping, and feeling, better.
Aim for 7-9 hours of sleep per night. Practice good sleep hygiene by going to bed at the same time each night, turning off electronics at least an hour before bedtime, and sleeping in a cool, quiet, dark, room.
Eliminate Toxins
A toxin is a poison — any substance that’s dangerous to the human body. That includes things you know are a problem such as heavy metals like lead, mercury, and cadmium, industrial chemicals and pollutants, and pesticides. It can also include common products you may not think of as being toxic, such as home cleaning products, body products, and even makeup. The best thing you can do to lighten your toxic burden is to prevent the toxins from getting into your system in the first place.
You may not have control over everything, yett you do have control over your own home. I focus my efforts on keeping my own home environment as clean as possible: I eat only organic food, filter my air and water, and use chemical-free products on my body and to clean my home. If your home is toxin-free, you’ll have a little bit more leeway when you go out into the environment. You can find out more about eliminating toxins on my blog.
Work Your Body
The science is irrefutable that exercise quite literally changes your genes. Exercise activates the brain’s growth hormone, BDNF, reverses memory decline in the elderly, and increases cell formation in the brain’s memory center. You can walk, jog or do yoga — anything you enjoy that gets you moving. All these brain benefits come from any form of aerobic exercise.
We tend to think of Alzheimer’s disease as a condition that afflicts the elderly suddenly. Enough evidence has surfaced that this is not true. This silent disease is very slow-moving, so you can stop it or even prevent it if you act now!
