Heart disease is commonly known as a “man’s disease.” However, heart disease kills 1 in 5 women each year. This fact is troubling and as a functional medicine physician I know it doesn’t have to be this way!
Heart disease in women is not a topic that is discussed as much as it should be and that needs to change. The truth is, heart disease in women is becoming more common despite increases in national heart health awareness. While the primary signs and symptoms of heart disease are similar for men and women, they are also very different. Sometimes women don’t recognize their signs as an indicator of heart disease.
Don’t worry! I’m going to tell you how you can recognize your risk factors, learn to identify the signs and symptoms, and give you the tools you need to advocate for your heart health. February is American Heart Month, so there’s no better time than NOW to take control of your heart health.
Heart Disease in Women vs Men
The biggest challenge in recognizing heart disease in women is that the symptoms are not as recognizable as they are in men because they don’t fit into the classic definition of heart disease made popular by conventional medicine.
Conventional medicine has a narrow list of factors before they consider someone at risk. The unfortunate part is that these risk factors for heart disease in women, which includes autoimmune disease, are overlooked because they can be tied to other diseases. I will discuss this as well as outline the symptoms of heart disease in women later in this article.
The symptoms and risk factors of heart disease in women aren’t the only differences between the sexes. While a man and a woman’s heart look similar there are considerable physical and functional differences. For starters, a woman’s heart is smaller than a man’s, as are some of the heart’s interior chambers. The walls of the chambers are actually thinner.
A woman’s heart beats faster than a man’s yet releases 10% less blood.1 A woman’s heart works harder with less! Another significant difference is how the heart responds to stress. When stressed, a woman’s heart beats faster and pumps more blood. However, when a man’s heart is stressed, the arteries constrict and his blood pressure increases.
Hormones also play an essential role in the differences in heart health and function in women. Men are more likely to suffer a heart attack before 55, whereas women’s hormones shift as they enter menopause and after. For most women, menopause is reached by the age of 55. The lower levels of estrogen after you’ve reached menopause puts you at higher risk for a heart attack.
The Risk Factors of Heart Disease in Women
The primary risk factors for heart disease in women are similar to those in men, such as high blood pressure, high LDL cholesterol (low-density lipoprotein cholesterol) and smoking. Remarkably, about half of everyone in the United States has at least one of these risk factors.2 I will discuss LDL cholesterol more in depth in just a minute as it’s a complex factor to be aware of.
It’s important to understand that one of the reasons there are exclusive risk factors for heart disease in women is because certain medical conditions only affect women. For example, only women can suffer from endometriosis, polycystic ovary disease, and diabetes and high blood pressure tied to pregnancy.3
Endometriosis is associated with chronic inflammation, heightened stress and plaque in the arteries. Studies have found that endometriosis increased the risk of heart disease in women by 400% in women under the age of 40.4
Aside from exclusive medical conditions, heart disease in women also increases due to:5
- Autoimmune diseases such as rheumatoid arthritis, which is more common in women than in men
- High testosterone levels during and prior to menopause
- Stress and depression – also more common in women
- And perhaps most importantly, lack of awareness of the above are risk factors
It is essential to know your risks so that you can take the steps to prevent heart disease.
The Impact of Oxidized LDL Cholesterol
Have you ever heard the story of that person that drops dead from a heart attack after their doctor tells them their cholesterol is fine? Even if your cholesterol levels are normal, you may still be at risk for heart disease.
While a routine lipid panel plays an important role in determining cardiovascular disease risk, it doesn’t provide a complete picture of your heart health. Conventional medicine doesn’t test oxidized levels of LDL cholesterol in a routine lipid panel.
Although high LDL cholesterol is considered a risk factor of heart disease in women and men, studies suggest that it does the most harm when the LDL cholesterol particle is small and oxidized.6The oxidation of LDL cholesterol is one of the first steps in development of inflammation in the artery.
The oxidation of LDL occurs when LDL cholesterol particles in your body react with free radicals; unstable molecules that are produced as a result of normal metabolism, a disease, or exposure to toxins. As a matter of fact, when we look at cholesterol markers, oxidized LDL (an oxidized lipoprotein that carries cholesterol) is one of the best markers of oxidative damage to your circulatory system, including inflammation in the artery wall. Recent evidence suggests that inflammation in the artery wall increases the risk of heart disease in women.7
You can reverse the damage of oxidized LDL by focusing on eating healthy fats such as avocado oil, wild-caught fish, or safflower oil, include plenty of fresh fruits and vegetables in your diet, and stay away from hydrogenated foods.8
Ask your functional medicine doctor to test your oxidized-LDL levels if you want to understand your risk for heart disease. I used Cleveland Heart Lab in my clinic to test my patients’ levels of oxidized LDL cholesterol, which is included in their inflammation testing panel.
The Autoimmune Link to Heart Disease in Women
Since autoimmunity and heart disease are linked, and autoimmunity disproportionately affects women, it’s important to dive into the link between autoimmune disease and heart disease in women.
Research suggests that people with certain autoimmune conditions have significantly higher rates of heart disease than the average population. Those with lupus, for example, have been shown to have a 4 to 8 times greater chance of developing heart disease. People with rheumatoid arthritis (RA), which is more common in women, not only have a reduced life expectancy, but heart disease is their leading cause of death.9
Often, it’s not the disease itself that increases risk of heart disease in women. It’s the medications used to treat autoimmune diseases, particularly steroids.10
Studies suggest that long-term use of corticosteroids can lead to obesity, insulin resistance, increased levels of cholesterol, and glucose intolerance.11 All of those side effects increase risk factors for heart disease.
Conventional medicine uses medication to manage symptoms which can lead to disease. That’s why it’s important to take a functional medicine approach and address the root cause of your autoimmune disease so that you can reverse it without increasing your risk of heart disease.
The Role of Menopause
Perimenopause and menopause are natural parts of a woman’s life that come with many changes and challenges.
Most people think of menopause as the time when a woman begins to transition out of her fertile period when she can conceive and bear children. However, that time is actually perimenopause.
During perimenopause, your ovaries’ production of estrogen and progesterone slows and eventually stops. This marks the end of your menstrual cycle. When you experience 12 months without a period, you have officially finished perimenopause and reached menopause. Perimenopause can begin in your 40s or 50s. Usually, it begins after age 45.
This drop in estrogen levels is believed to be a factor in the increased risk of heart disease in women.12
Studies suggest that estrogen plays a positive role in heart health by helping keep blood vessels flexible, which reduces stress on the artery wall so it can expand to accommodate blood flow.13 As estrogen levels drop, blood vessels may become stiff and rigid leading to an increase in blood pressure.
Your cholesterol levels may also change as a result of the decreased production of estrogen, leading to an increased risk of heart disease in women. As a result of these changes, you may be more prone to atrial fibrillation, an irregular, often rapid, heart rate that causes poor blood flow. Atrial fibrillation can lead to more serious heart conditions.14
Now that you understand the role menopause plays in heart disease in women, it is even more critical to know all of your risk factors for heart disease, especially as you near the age of perimenopause. That way you can take control of your heart health and prevent heart disease.
 Dr. Amy Myers
February 15th, 2021
https://content.amymyersmd.com/article/heart-disease-and-women/Early Warning Signs Of Heart Disease In Women – Infographics – Amy Myers MD®
Dr. Amy Myers
February 15th, 2021
https://content.amymyersmd.com/article/heart-disease-and-women/Early Warning Signs Of Heart Disease In Women – Infographics – Amy Myers MD®Symptoms of Heart Disease in Women
Before I talk about the symptoms of heart disease in women, it’s important to understand the difference between heart disease and a heart attack. A heart attack is a medical emergency that requires immediate medical attention. Heart disease refers to several types of heart conditions and can eventually lead to a heart attack if left untreated.
Common heart disease symptoms such as chest pain can occur in both men and women. However, recent evidence indicates that women may experience different — and in some cases milder — symptoms of heart disease than men.
Men are more likely than women to experience chest pain as a symptom of heart disease.15
That doesn’t mean women experience chest pain less than men. Sometimes women don’t recognize they are having chest pain! There is scientific evidence that women have a higher tolerance for pain than men, which could lead women to disregard chest pain because it is not severe. Or, the chest pain may be so mild they don’t feel pain at all.16
Chest pain is one of the more common symptoms of heart disease in both sexes, however many women may not show any symptoms of heart disease until they have a heart attack.
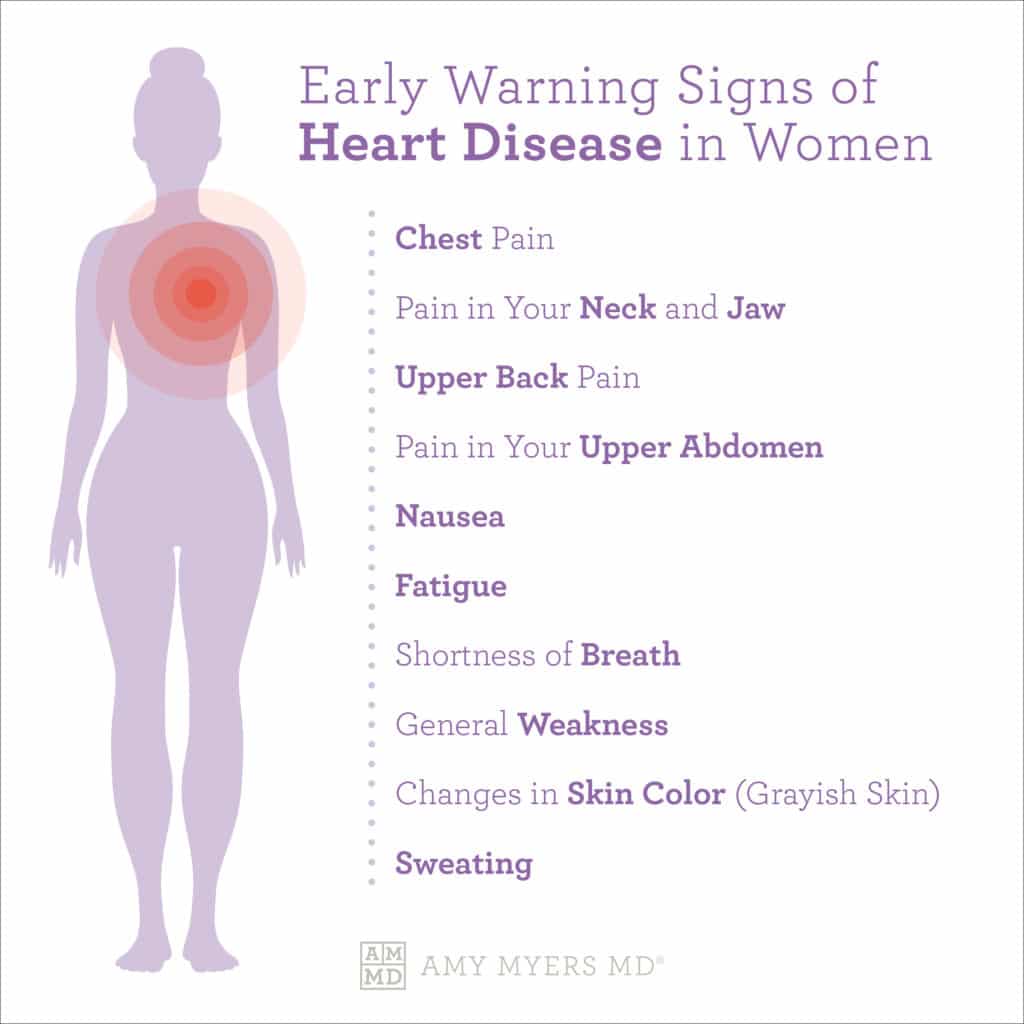
However, there are early signs of heart disease that women experience but may not recognize as warning signs, including:17
- Pain in your neck and jaw
- Upper back pain
- Pain in your upper abdomen
- Nausea
- Fatigue
- Shortness of breath
- General weakness
- Changes in skin color, such as grayish skin
- Sweating
These symptoms of heart disease in women can occur while you are at rest or being active. They can also be symptoms of a heart attack so knowing your body and understanding when something is wrong and advocating for yourself is critical.
How to Lower the Risk of Heart Disease in Women
It’s never too late to take care of your heart and lower your risk of heart disease. Now that you have a better understanding of your risk factors and symptoms, I recommend following five steps to help support healthy heart function and optimize your cardiovascular health.
1. Optimize Your Diet
Your diet is one of the top contributors to heart health. A diet high in processed foods, refined sugars, and unhealthy fat will do tremendous damage to your heart. That’s why it’s important to eat a nutrient-dense diet and eliminate toxic and inflammatory foods. Here are some nutrient rich foods I suggest to lower the risk of heart disease in women:
- Wild-caught fatty fish such as salmon
- Green leafy vegetables
- Healthy fats such as avocado, olive oil, almonds, pecans, and walnuts
- Foods high in magnesium such as spinach and walnuts
- Berries
- Dark chocolate
Your body doesn’t naturally produce fatty acids like omega 3, so it’s important to get these vital nutrients through food. Foods such as wild-caught salmon contain high levels of omega-3s, which support a healthy blood flow and viscosity and can support an optimal hormonal balance.
2. Reverse your Autoimmunity
As we discussed earlier, autoimmunity and heart disease are closely linked and inflammation is a major driver of autoimmune disease. The good news is that you CAN reverse your autoimmunity. By following The Myers Way®, my simple and proven dietary and lifestyle protocol, you can reclaim your health by addressing the true underlying causes of autoimmune disease. I have seen the success of this protocol firsthand, in my clinic and as a patient myself, and now people everywhere can benefit from this medical breakthrough.
3. Relieve Your Stress
Relieving your stress in a global pandemic isn’t the easiest thing to do. Struggling with work-life balance and our constant connection to technology makes things even more difficult.
Our stress response evolved primarily as a means of self-preservation from our ancestors facing immediate, life-threatening situations. Unfortunately, that response isn’t ideal for the type of chronic, ongoing stress we face today. That’s why it’s so crucial to make time to de-stress!
Some of my favorite stress-reducing activities include:
- Meditation and breathing exercises – I recommend the app HeartMath
- Going for a hike with my family – getting some fresh air and physical activity is key
- Sweating and detoxing in my infrared sauna
- Laughing and playing with my daughter Elle – it’s true that laughter is the best medicine
4. Balance Your Hormones Naturally
Hormones affect your body temperature and heart rate, your mood, your appetite, your sex drive, growth and development, and more. As I mentioned earlier, when you reach perimenopause, your estrogen levels decrease. The absence of this hormone has been linked to an increased risk of heart disease in women.
Hormone replacement therapy is often used to treat the decreased levels of estrogen during menopause. However, there’s still some debate over whether or not hormone replacement therapy benefits your heart health or offers no benefits.
A study conducted by the Women’s Health Initiative found that there were no benefits from hormone replacement therapy, and that women given synthetic hormone replacement therapy showed a slight increase for stroke and blood clotting. If you’re experiencing symptoms, I recommend discussing non-synthetic hormone therapy with your functional medicine doctor or considering natural solutions.
5. Support Your Heart Health
CoQ10 and activated B vitamins support healthy cholesterol levels, circulation, and vascular health and neutralize oxidative damage from free radicals.mCoQ10 is a heart-supporting enzyme and free radical fighter. This enzyme is naturally found in organ meats such as sardines and grass-fed beef liver, yet the levels in these foods are relatively low.
Now that you have the tools necessary to take control of your heart health, don’t wait. Take these simple steps today to achieve optimal health. Increasing your knowledge, making lifestyle changes, and supporting your heart health is the best defense against heart disease in women.
Article Sources
- Women or Men — Who Has a Higher Risk of Heart Attack?. Leslie Cho, MD. Cleveland Clinic. 2020.
- Risk Factors for Heart Disease. Janet M. Torpy, MD. Jama . 2003.
- Women or Men — Who Has a Higher Risk of Heart Attack?. Leslie Cho, MD. Cleveland Clinic. 2020.
- Women or Men — Who Has a Higher Risk of Heart Attack?. Leslie Cho, MD. Cleveland Clinic. 2020.
- Heart Disease: Differences in Men and Women. Dr. Lili Barouch. Johns Hopkins Medicine . 2019.
- Association Between Circulating Oxidized LDL and Atherosclerotic Cardiovascular Disease: A Meta-analysis of Observational Studies. Shen Gao, MD; Dong Zhao, MD, PhD; Miao Wang, MD; Xueyu Han, MD; Yue Qi, MD, PhD; and Jing Liu, MD, PhD. Canada Journal of Cardiology. 2017.
- The Science of Oxidized LDL Cholesterol and inflammation. Cleveland Heart Lab. 2020.
- The Danger of Oxidized Cholesterol and Tips for Prevention. Brian Wu, PhD. Heartline. 2018.
- Accelerated Atherosclerosis in Autoimmune Rheumatic Diseases. Yehuda Shoenfeld, Roberto Gerli, Andrea Doria, Eiji Matsuura, Marco Matucci Cerinic, Nicoletta Ronda, Luis J. Jara, Mahmud Abu-Shakra, Pier Luigi Meroni, and Yaniv Sherer. AHA Journals. 2005.
- Prednisone and other corticosteroids. Mayo Clinic. 2020.
- Corticosteroid Adverse Effects. Muhammad Yasir; Amandeep Goyal, Pankaj Bansal, and Sidharth Sonthalia. NCBI. 2020.
- Menopause and Heart Disease. American Heart Association. 2015.
- The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Andrea Iorga, Christine M Cunningham, Shayan Moazeni, Gregoire Ruffenach, Soban Umar, Mansoureh Eghbali. PubMed. 2017.
- Cardiovascular health and the menopausal woman: the role of estrogen and when to begin and end hormone treatment. Frederick Naftolin, Jenna Friedenthal, Richard Nachtigall, and Lila Nachtigall. NCBI. 2019.
- Women with myocardial infarction are less likely than men to experience chest symptoms. Mona Løvlien, Berit Schei, and Torstein Hole. PubMed. 2006.
- Male-Specific Conditioned Pain Hypersensitivity in Mice and Humans. Loren J Martin, Erinn L Acland, Chulmin Cho, Wiebke Gandhi, Di Chen, Elizabeth Corley, Basil Kadoura, Tess Levy, Sara Mirali, Sarasa Tohyama, Sana Khan, Leigh C MacIntyre, Erika N Carlson, Petra Schweinhardt, and Jeffrey S Mogil . PubMed. 2019.
- What You Need to Know About Heart Disease in Women. Erica Hersh . Heartline. 2019.
