What Is Inflammatory Bowel Disease
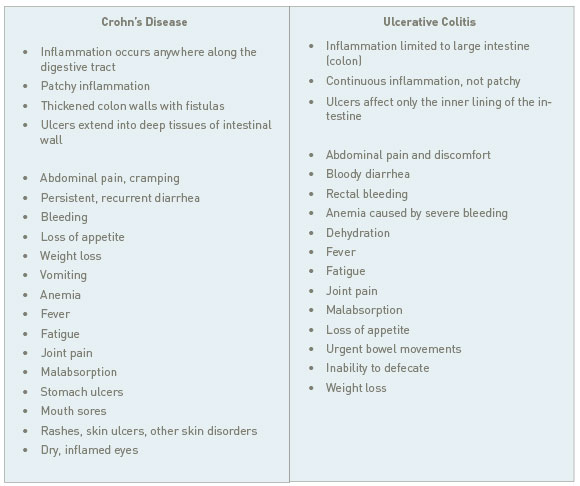
Inflammatory Bowel Disease, or IBD, is a group of inflammatory conditions affecting the intestines and colon. The two main forms of IBD are ulcerative colitis and Crohn’s disease—two diseases that, despite falling under the umbrella of IBD and sharing many symptoms, are actually quite different.
Distinguishing between Crohn’s disease and ulcerative colitis allows me to choose the most effective strategy for each patient. The location of the inflammation, the specific symptoms, and the possible causes are all clues that can eventually lead to a solution.
 Dr. Amy Myers
February 6th, 2015
https://content.amymyersmd.com/article/inflammatory-bowel-disease/Inflammatory Bowel Disease – Comparing Chron’s Disease and Ulcerative Colitis – Infographic – Amy Myers MD®
Dr. Amy Myers
February 6th, 2015
https://content.amymyersmd.com/article/inflammatory-bowel-disease/Inflammatory Bowel Disease – Comparing Chron’s Disease and Ulcerative Colitis – Infographic – Amy Myers MD®By the time symptoms have begun, conventional medicine treats both diseases in much the same way: with a slew of immunosuppressive medications and invasive surgeries. By ignoring the upstream factors that led to the disease, these methods don’t address the thing that caused the inflammation in the first place. As time goes by, IBD symptoms can reach beyond the gastrointestinal tract, even involving the eyes, joints, and skin.
Causes of Inflammatory Bowel Disease
Crohn’s disease and ulcerative colitis are considered idiopathic, meaning their causes are unknown. They aren’t officially classified as autoimmune diseases, but share some of the same risk factors (what I call the “pillars” of autoimmunity):
- Pillar I: Leaky Gut
- Pillar II: Diet
- Pillar III: Toxins
- Pillar IV: Infections and Stress
In my clinic, I start by with these four factors. I heal the gut, clean up the diet, and address any toxins, infections, and stress that could be driving inflammation. But there are certain things I’ve found to work better in Crohn’s disease, and not as well in ulcerative colitis (and vice versa).
Inflammatory Bowel Disease – What You Need to Know
Gut Infections Could Be the Culprit
SIBO and candida overgrowth are common problems in both Crohn’s disease and ulcerative colitis. A malfunctioning gastrointestinal tract decreases your ability to clear yeast, bacteria, and bacterial debris from your system. As these microorganisms overpopulate, they excite your immune system and cause further damage to your gut.
In Crohn’s disease, deep ulcers and fistulas create pockets where bacteria and yeast can flourish. You may need prescription medications to clear a particularly stubborn infection in the beginning, supplementing with plant enzymes like caprylic acid, candifense, and microb-clear.
Not All Parasites Are Created Equal
In our hyper-hygienic modern world, nobody likes the idea of living with parasites. I routinely screen my IBD patients for intestinal parasites with a stool test. But before I help them clear the infection, I assess whether or not the parasite is a) directly harmful, or b) potentially beneficial. That depends on the type of parasite and the type of IBD.
In ulcerative colitis, parasites can actually cause the condition. Amoebic colitis, which is caused by a protozoa, produces many of the same painful symptoms as ulcerative colitis and is hard to distinguish. Clearing the infection with medications and supplementing with anti-parasitic herbs can sometimes be enough to reverse symptoms.
But parasites are not a common cause of Crohn’s disease—in fact, some Crohn’s treatments involve the introduction of certain parasitic worms called helminths into the gastrointestinal tract to reduce symptoms. Helminths, such as hookworms and whipworms, have anti-inflammatory and immune-modulating effects that have been shown to reduce symptoms of Crohn’s. Many researchers suspect this is because of the “hygiene hypothesis.” The idea is that the industrialized world is too clean, and that we are no longer exposed to the common pathogens that our immune systems used to encounter generations ago.
Different Diseases Need Different Diets
In general, I recommend that all of my patients avoid certain foods that are just downright inflammatory, especially in the beginning when your gut is so inflamed. This includes gluten, dairy, and grains. If you have any form of IBD, minimize the sugar content of your diet to reduce yeast and bacteria overgrowth, which is so often a culprit.
I’ve found that the protein content of a patient’s diet really makes the difference. A higher protein diet, like a Paleo-type diet or the Specific Carbohydrate Diet (SCD) works well for people with Crohn’s disease, but those with ulcerative colitis usually respond better to a diet with less protein. A high-fiber diet that contains a lot of omega-3s (from fish, for example) is the ideal diet for someone with ulcerative colitis.
