Are you battling with stubborn and recurring Candida overgrowth? Did you know that could be due to your infant gut health? While your diet and lifestyle choices greatly influence your gut health, the foundation for your gut microbiome began developing when you were a fetus in the womb from the nutrients passed from your mother. Unfortunately, that may have also included bad bacteria.
If born vaginally, we receive even more protective bacteria through the journey out of the birth canal. However, along with a beneficial microbiome, it’s possible to inherit imbalanced amounts of bacteria as well. This is especially true for babies born via cesarean section (C-section), whose first exposures to bacteria are from skin, mouths, and medical tools. In these cases, the infant microbiome starts out at a disadvantage, leaving them vulnerable to Candida overgrowth as an adult.
The truth is, your infant gut health has such a greater influence over your adult gut health than you realize. I will discuss the link between Candida and your infant gut health, how you could have been exposed to Candida as a child, and how to maintain a healthy gut microbiome. First, let’s have a refresher on what Candida is and why it overgrows.
What is Candida?
Candida is a fungus, a type of yeast, that lives in your mouth and intestines in small amounts. Its job is to aid with digestion and nutrient absorption. It is a part of your body’s normal microflora — the microorganisms that live in a delicate balance in your mouth, throat, gut, vagina in women, and on your skin.
Ideally, your good bacteria, bad bacteria, and Candida (among other forms of yeast, viruses, and even mites) that make up your gut microbiome exist in a balanced state. In fact, I like to think of your microbiome as a rainforest, with many different species living together in harmony.
When one species gets out of balance in your rainforest, everything gets out of control. When this balance is tipped between Candida and other microorganisms, Candida overgrowth occurs.
Candidiasis, or yeast overgrowth, is very common and causes Candida overgrowth symptoms such as bloating, constipation, rashes, fungal infections, fatigue, brain fog, and mood swings.
The healthy or ‘good’ bacteria in your gut typically keep your Candida levels in check. However, the yeast population can get out of hand if a round of antibiotics kills too many of the friendly bacteria or you have a diet high in refined carbohydrates and sugar (which feed the Candida.)
High alcohol intake, oral contraceptives, and a number of other factors including a high-stress lifestyle can also cause Candidiasis. Even a diet rich in fermented foods like Kombucha, sauerkraut, and pickles can feed Candida.1
Signs of Candida Overgrowth
Because yeast overgrowth can become a full-body problem, Candida symptoms can be experienced in many different forms nearly anywhere in the body. Some of the most common signs and symptoms of Candida overgrowth are:
- Brain fog
- Leaky gut
- Autoimmunity
- Fatigue, chronic fatigue, fibromyalgia
- Gas and bloating
- Diarrhea or constipation
- Sugar cravings, weight gain, or difficulty losing weight
- Diabetes
- Skin issues (acne, rosacea, eczema, psoriasis, tinea versicolor)
- Dry, itchy, or red skin
- Nail fungus, athlete’s foot, dandruff
- Recurring yeast infections
- Vaginal, rectal, or jock itching
- Itchy ears
- Mood swings, sleep issues, anxiety, or depression
- Sinus infections or seasonal allergies
- Severe seasonal allergies
The Link Between Candida and Pregnancy
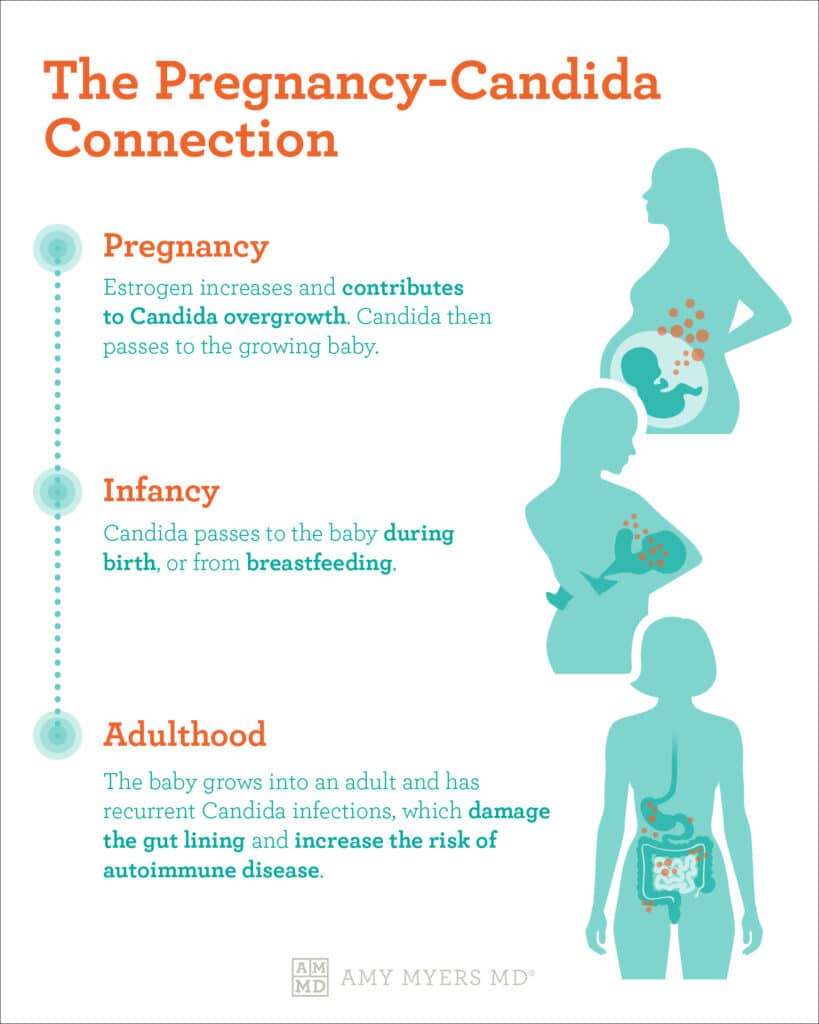
When you were pregnant, did you develop vaginal yeast infections? Higher than usual levels of estrogen disrupt the body’s pH levels (the balance between acid and bases), leaving your gut microbiome vulnerable to Candida overgrowth.2
Estradiol, a form of estrogen released in large amounts during pregnancy, is vital in growing the womb’s muscle layer and initiating labor.3
 Dr. Amy Myers
October 31st, 2021
https://content.amymyersmd.com/article/infant-gut-health/The Pregnancy-Candida Connection – Infant Gut Health – Infographic – Amy Myers MD®
Dr. Amy Myers
October 31st, 2021
https://content.amymyersmd.com/article/infant-gut-health/The Pregnancy-Candida Connection – Infant Gut Health – Infographic – Amy Myers MD®The spike in this protective hormone, however, fosters an environment perfect for Candida overgrowth. Additionally, the fungus binds to minerals such as iron, zinc, and magnesium – all nutrients your body is likely getting more of between prenatal vitamins and an increased food intake.4 This fungus can be passed on to the fetus, therefore disrupting infant gut health.
The same principle applies to those taking birth control or traditional hormone replacement therapy. If you’ve ever taken these medications, your higher estrogen levels left you more susceptible to yeast infections driven by Candida overgrowth.
If you’re going through menopause or taking birth control and suffering from the effects of estrogen in overdrive, it’s worth exploring ways to manage symptoms. And it’s why I developed Adrenal Support for not only relieving menopausal symptoms but also supporting a healthy menstrual cycle without causing high estrogen levels.
Candida, Birth, and Infant Gut Health
As I mentioned, pregnancy and your infant gut health is the foundation for your gut health as an adult. So, just how much influence does your infant gut health have? As it turns out, a lot!
Early exposure to Candida in utero, inside the vaginal canal, or shortly after birth can lead to recurring Candida overgrowth as an adult. The chances of your exposure as an infant increase if Candida was passed through breastfeeding or if you were given antibiotics after birth. These antibiotics disrupt an already vulnerable infant microbiome.
The Infant Microbiome
Historically, the breastfeed infant microbiome was a monoculture of the bacteria bifidobacterium, a bacteria that does not need oxygen to grow.5
This promoted healthy infant gut microbiome development to allow all the microorganisms to live in harmony. Formula-fed infant microbiomes were much more diverse with more microbes than bifidobacterium, allowing exposure to harmful bacteria and microbes.
Modern or conventional farming methods that involve the use of genetically modified organisms (GMOs), synthetic fertilizers, pesticides, and herbicides simply did not exist back then. These chemicals can be passed through a mother’s breast milk, which disrupts the infant gut microbiome allowing more microbes to enter, including Candida.
This Candida can grow out of control. In fact, it’s a rather clever species of fungi. Candida cells can penetrate the single-cell layer of your infant gut microbiome by changing their shape. Under certain conditions, typically round cells transform to an elongated, stick-like cell shape, evolving to pierce holes in the gut wall and allowing toxins to pass through.6
A Candida-infested infant microbiome can lead to a suppressed immune system as an adult, leading to autoimmune disease. I’ll discuss more about the long-term effects of Candida and infant gut health later. First, let me tell you how the way you were born impacted your infant gut health.
C-Sections, Vaginal Seeding, and Infant Gut Health
The World Health Organization states that c-sections are medically necessary in 10% to 15% of all pregnancies. Sometimes having a C-section is unavoidable and that’s perfectly acceptable. However, having a c-section has a great impact on infant gut health.
Babies born by a c-section aren’t getting exposed to the microbiota and their genetic material, the infant gut microbiome.7
These microbial cells are passed on to babies in the vaginal canal and live with humans from birth. They are essential for optimal health.
In 2019, the largest study was performed on the infant gut microbiome. The study analyzed nearly 600 births in the United Kingdom and looked at the presence of bacteria and microbes in babies. The results found that babies born by c-sections lacked strains of healthy bacteria found in healthy individuals compared to those born vaginally.8 Instead, babies born by c-section had more opportunistic bacteria that disrupted the infant gut microbiome. Don’t worry, there are solutions if you cannot avoid having a C-section.
A common practice performed on babies born by a C-section is vaginal seeding. After birth, a doctor swabs the vaginal fluids with a cotton swab and transfers it to the nose, mouth, or skin of the newborn. Its purpose is to allow for the colonization of the infant gut microbiome to reduce the risk of long-term effects such as Candida overgrowth and the development of autoimmune diseases.9
It’s important to advocate for your health and your baby’s health with your doctor. Take notes and stick with your birthing plan, unless you need to waiver from it for medical reasons.
Lasting Effects of Infant Gut Health & Candida
As I’ve discussed, your infant gut health impacts your gut health for the rest of your life. If you were exposed to bad bacteria and did not receive the microbiota during birth that lives in the vaginal canal, your gut could be susceptible to infection as an adult, including Candida overgrowth.
In my decades of practice as a doctor and working with thousands of patients, I’ve found Candida overgrowth, paves the way for leaky gut, which opens the door for you to develop an autoimmune disease, or two.
A leaky gut opens the door for toxins, undigested food particles, bacteria, and viruses to pierce your intestinal wall and infiltrate your bloodstream. Your immune system prompts an inflammatory response in an attempt to fight off these foreign invaders, and in the process becomes overworked. Eventually, your weakened immune system gets confused and works less efficiently, often turning on its own body tissues via a full-blown autoimmune disorder.
The good news is that you can fight back!
How to Treat Candida Overgrowth
Treating Candida overgrowth doesn’t just involve stopping the growth. It also means restoring the friendly bacteria that usually keep them in check. The final step is repairing your gut so that the Candida overgrowth can no longer enter your bloodstream. I accomplish this with a simple three-wave attack:
Step 1: Starve the Candida
Once you’ve identified a Candida outbreak, you can start the process of regaining bacterial balance by starving Candida cells. This means cutting all sugar and alcohol from your diet. I also recommend temporarily limiting carbohydrates such as fruit, starchy vegetables, grains, and legumes.
Candida feeds on toxic and inflammatory foods, which is why it’s especially important to cut sugar and alcohol from your diet in order to starve its source of growth. Eliminating these foods from your diet should go hand in hand with increasing intake of foods that minimize Candida growth, like coconut oil, garlic, cloves, cinnamon, and wild-caught seafood.
Step 2: Attack the Candida
Next, you’ll want to attack the Candida by taking supplements that help break down the cell wall of yeast cells. I use Candifense® as well as Caprylic Acid. Candifense® supports microbe balance in the GI tract and discourages the growth of yeast while Caprylic Acid helps penetrate intestinal mucosal cells to exert the effect of yeast. Both Candifense® and Caprylic Acid are excellent at helping to break down the walls of Candida cells.
Step 3: Repopulate the good bacteria in your gut.
Finally, you will repopulate your gut with good bacteria using a high-potency probiotic to keep Candida under control. While battling Candida overgrowth, I recommend a probiotic supplement containing 100 billion colony-forming units (CFUs) to restore your gut’s healthy microbial balance. Probiotics will help restore the natural balance of bacteria in your gut and prevent Candida overgrowth from recurring.
If you suffer from repeated Candida overgrowth, you likely can trace it back to your infant gut health. The good news is that you can do something about it. Following the three steps above can help you get rid of the overgrowth and balance the bacteria in your gut microbiome.

Article Sources
- Systemic candidiasis: a study of 109 fatal cases. W T Hughes. Pediatric Infectious Disease vol. 1,. 1982.
- Why Pregnant Women Are More Prone to Yeast Infections. Rachael Rettner. Live Science. 2016.
- What does Estradiol do?. Dr. Ananya Mandal, MD. Medical Life Sciences. 2019.
- A Patient’s Guide to Candida in Pregnancy. Sacred Vessel Acupuncture & Functional Medicine. 2019.
- Bifidobacteria and Their Role as Members of the Human Gut Microbiota. Amy O'Callaghan and Douwe van Sinderen. Frontiers in Microbiology. 2016.
- Growth of Candida albicans hyphae. Peter E. Sudbery. Nature Reviews Microbiology. 2011.
- What are the gut microbiota and human microbiome?. Saurabh Sethi, M.D., MPH . Medical News Today. 2018.
- C-section babies are missing key microbes. Ewen Callaway. Nature Reviews Microbiology. 2019.
- Vaginal Seeding. Committee on Obstetric Practice. The American College of Obstetrics & Gynecologists. 2017.
