Screening for colon polyps provides vital insight into the health of your digestive system and early detection of colon cancer. Yet, do you know when to get a colonoscopy?
I had a colonoscopy in November, and I’m here to tell you there is nothing to worry about when getting a colonoscopy. You’re not awake during the procedure and don’t feel anything. Yet, many people avoid getting a colonoscopy. In fact, The Centers for Disease Control and Prevention (CDC) estimates that 1 in 3 adults between the ages of 50 to 75 have never had a colonoscopy.1
Colon cancer is one of the most prevalent types of cancer in the United States. Yet, it doesn’t have to be this way. Colon cancer is preventable, and screening for colon polyps with a colonoscopy is vital to early detection.
I will tell you about colon polyps, why we develop them, and functional medicine’s approach to preventing them from forming in the first place. First, let’s discuss when to get a colonoscopy.
When Should You Get a Colonoscopy?
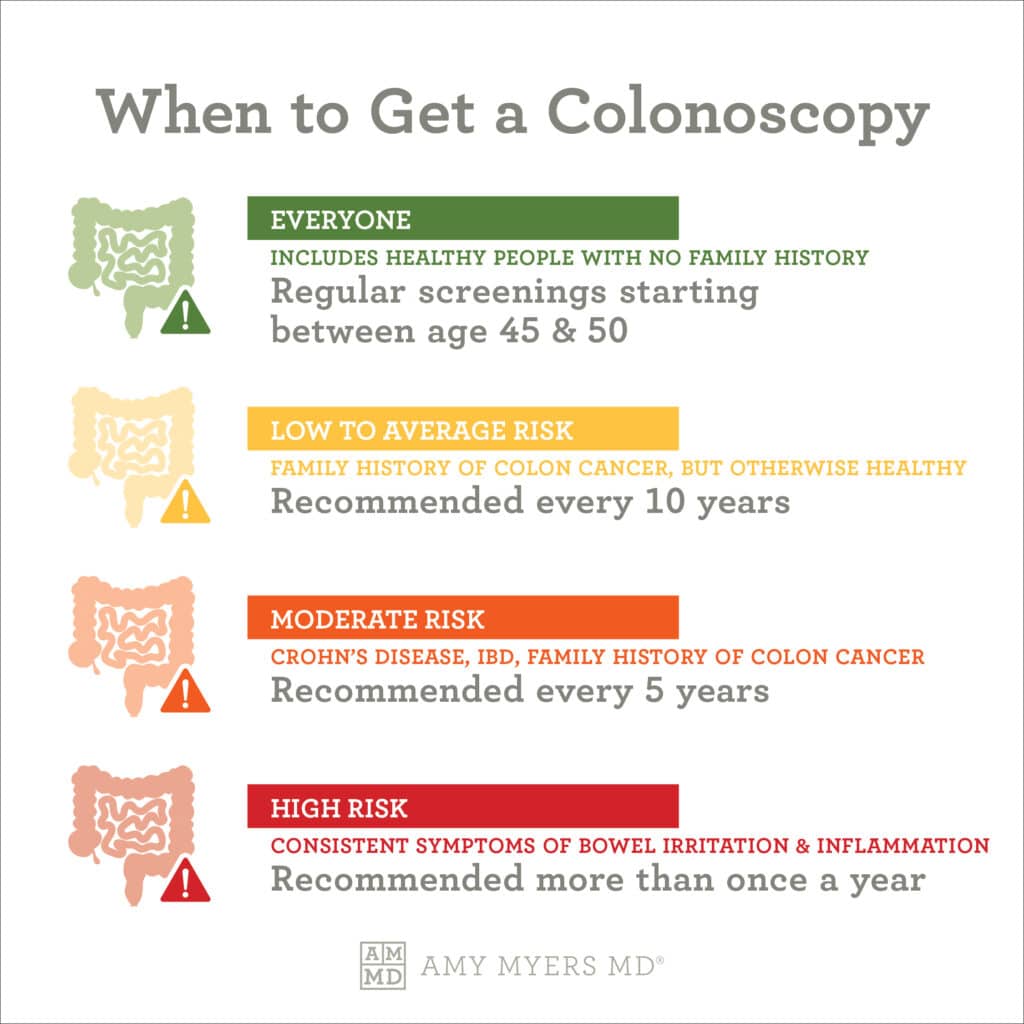
Regular screenings for colon polyps can find them when they are small, haven’t spread, or before they turn into cancer. Colonoscopies also can detect Crohn’s disease, diverticulitis (inflammation of the bowel), and inflammatory bowel disease (IBD).
In the past, it was recommended that anyone between 50 and 75 years old have a regular colonoscopy screening. The American Cancer Society recently lowered that recommendation to 45 because of the increased rates of colon cancer among people younger than 50.2
If you have an average risk of developing colon cancer or have no family history, the ACS recommends:
- Start regular screenings at age 45
- If you are in good health, you should have routine screenings every 10 years until age 75.
- People between 76 and 85 should talk to their doctor about whether to get screened or not.
- If you are over 85, you no longer need to be screened.
If you are at a higher risk, the ACS recommends that screenings may need to start before age 45 and may need screenings more often or get more in-depth testing. I’ll talk about some tests we use in functional medicine later.
A person of high risk is anyone with a family or personal history of colon cancer or someone with a history of IBD or Crohn’s disease. You should talk to your doctor if you are at high risk.
 Dr. Amy Myers
January 29th, 2023
https://content.amymyersmd.com/article/when-to-get-a-colonoscopy/when to get a colonoscopy – infographic – Amy Myers MD®
Dr. Amy Myers
January 29th, 2023
https://content.amymyersmd.com/article/when-to-get-a-colonoscopy/when to get a colonoscopy – infographic – Amy Myers MD®Prepping for a Colonoscopy
The preparation was the most challenging part for many people and me. Everyone I talked to as I got ready for my first routine colonoscopy told me the preparation was the most difficult part.
One of the important ways to ensure a successful colonoscopy is to empty the contents of your bowels. If you haven’t done the prep work, polyps and lesions can be missed during the colonoscopy procedure, or it may take longer.
I began by eating a low-fiber diet a few days before, which meant I couldn’t eat whole grains, nuts, seeds, dried fruit, or raw fruits and vegetables. Note: I don’t eat whole grains because they contain gluten, which is highly inflammatory for most people. If you follow an autoimmune diet (AIP), seeds and nuts are not allowed.
The day before my colonoscopy, I was on a completely liquid diet of Bone Broth Collagen, Roar Peach Water, and Flow Alkaline Spring Water, to which I added Collagen Protein. I was also prescribed by my doctor the Suprep® Bowel Prep Kit.
Collagen helps rebuild your gut lining and supports the digestion process. If you’re preparing for a colonoscopy, I highly recommend supplementing with Collagen Protein.
My first meal after my colonoscopy was gluten-free almond crackers and gluten-free pumpkin bread because these foods are easy to digest. I also took Acetyl-Glutathione to detox my body and remove the Propofol used to put me to sleep for the procedure. Glutathione is a supercharged boost for your body’s most potent detoxifier.
Now that you know when to get a colonoscopy and how to prepare for them. Let’s discuss what they are looking for– colon polyps.
What are Colon Polyps?
A colon polyp is a small clump of cells that forms in the line of colon. Most of these polyps are harmless and can go away on their own. However, some polyps turn into colon cancer. Anyone can develop colon polyps. However, you are at a higher risk after the age of 50, are overweight or a smoker, or have a personal or family history of colon cancer.
As I mentioned, if caught early they can be removed safely and completely. I’ll talk about how to make your gut inhospitable for colon polyps and reduce your risk of developing colon polyps in just a bit. Let’s talk about what causes colon polyps.
Causes of Colon Polyps
Earlier I mentioned that age, family history, and lifestyle increase your risk of developing colon polyps. Other risk factors include smoking and excess alcohol use, obesity, or a sedentary lifestyle.3
There are two types of polyps: non-neoplastic polyps and neoplastic polyps. Neoplastic polyps are more likely to become cancerous. Non-neoplastic polyps are not likely to become cancerous. The three types of non-neoplastic polyps are:4
- Inflammatory Polyps
- Hyperplastic polyps
- Hamartomatous polyps
Inflammatory polyps often occur in people with inflammatory bowel disease, while hyperplastic polyps develop where the body has repaired damaged tissue.
Food is a huge factor in your increased risk of developing colon polyps. Fatty foods, highly processed foods, and processed meat such as deli meats, hot dogs, bacon, and sausage can make your gut a habitable place for polyps to develop. I will tell you about the functional medicine approach to preventing colon polyps.
The Functional Medicine Approach to Colon Polyps
In functional medicine, we want to get to the root cause of what’s causing the polyps to develop. It starts inside your gut microbiome.
A healthy gut microbiome consists of a balance of beneficial and harmful bacteria. Each strain of bacteria affects various body parts and can influence such diverse factors as weight, cognitive function, immune health, and a host of other functions. Yet, the “bad” bacteria can outnumber the “good” bacteria due to a leaky gut, infection, stress, poor diet, and environmental toxins.
A leaky gut allows bacteria and toxins to spread into your body, causing various health problems. For example, leaky gut can lead to inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), ulcerative colitis, and Crohn’s disease.
Leaky gut can also lead to an imbalance or “dysbiosis” in your gut, negatively impacting the good bacteria that are naturally there and affecting your overall health since 80% of your immune system lives in your gut.
The first step to preventing colon polyps is healing your gut by providing the nutrients it needs. Leaky Gut Revive® supports a healthy gut microbiome by preventing and healing leaky gut. It offers an excellent source of L-glutamine to nourish your gut cells, aloe extract to help restore your gut’s mucosal lining, licorice extract to soothe the stomach and intestinal lining, and larch arabinogalactan to promote healthy microflora in your gut microbiome.
Leaky Gut Revive® is my No. 1 tool for repairing a leaky gut. Once you’ve addressed your leaky gut, the next step is to create an uninhabitable environment for polyps to develop. Let me tell you how to do that.
How to Make an Uninhabitable Environment for Polyps
To promote the balance of bacteria in your gut microbiome, your microbiome needs a postbiotic called butyrate. You’ve probably heard me talk about the importance of taking a daily probiotic and prebiotics.
To review, probiotics are living microorganisms that can work in your gut to support your body in many ways. They can be found in dietary supplements and fermented foods, as well as within the natural microbiome of your body.5
Prebiotics are dietary fibers from carbohydrates that bypass digestion to get into your colon. Once in your colon, the microorganisms metabolize and ferment the prebiotics to survive, which creates a variety of byproducts to support your gut health.
Postbiotics, such as butyrate, are naturally produced when probiotics feed off prebiotics. Butyrate is a short-chain fatty acid that controls inflammation, provides energy to your cells that make up your gut-lining, and keeps your gut microbiome in balance. Butyrate also plugs up a leaky gut and can help you lose weight.6 Let me tell you how to promote your body’s natural production of butyrate.
A Doctor’s Solution to Promoting Butyrate Production
If butyrate forms when prebiotics feed probiotics, combining a probiotic and a prebiotic would make sense. A high-fiber diet is essential to promote healthy bowel patterns and colon health.
I created Prebiotic Fiber Complete™ to include multiple types of fiber and specific prebiotics to help you achieve optimal digestive health, including Fibriss™ and Inulin. I also included Fibregum™ when formulating Prebiotic Fiber Complete™ to feed the many beneficial strains of bacteria in your digestive tract, improving digestion and strengthening your body’s natural immune response.
Prebiotic Fiber Complete™ is a physician-formulated fiber blend to give the good bacteria in your gut the strength it needs to fight off the overgrowth of harmful bacteria. When you add a prebiotic to a daily probiotic, you give your gut a strong army for optimal digestive health!
How to Choose a Prebiotic?
Probiotic supplements are sold in different strengths called CFUs (colony-forming units). The CFU tells you how many bacteria are within that particular probiotic. When searching for the best probiotic, consider the number of CFUs.
Probiotic Capsules 100 Billion is designed for maximum support. You won’t see very many products on your local store shelves that have this potency level AND don’t need to be refrigerated. Probiotic Capsules 30 Billion is available for those who can not tolerate a high level of probiotics and provides an excellent maintenance dose.
Because SIBO is an overgrowth of bacteria in the small bowel often caused by chronic constipation or challenges with the nervous system, adding more lactic acid-based bacteria into the small intestine can often add more fuel to the fire.
This is why I recommend Primal Earth Probiotic to anyone with SIBO, who suspects SIBO may be at the root cause of their issues, or simply doesn’t tolerate most probiotics.
The Final Word on When to Get a Colonoscopy
Creating an uninhabitable environment for colon polyps to develop by repairing your gut, eating a high-fiber diet, and providing your gut with probiotics and prebiotics to promote butyrate production is a way to prevent the development of colon polyps.
Colon cancer is one of the most common types of cancer. A colonoscopy is an excellent tool for early detection. Talk to your functional medicine doctor about when to get a colonoscopy.
Article Sources
- Colorectal cancer screening rates remain low. Centers for Disease Control and Prevention. 2021.
- When Should You Start Getting Screened for Colorectal Cancer?. American Cancer Society. 2021.
- Colon polyps. Mayo Clinic. 2021.
- What Causes Colon Polyps?. Compas Onctology. 2022.
- Probiotics: What You Need To Know. National Center for Complementary and Integrative Health. 2022.
- The Health Benefits and Side Effects of Butyrate. Cleveland Clinic. 2022.