Have you laid in bed at night exhausted, yet unable to go to sleep because you constantly have the urge to move your legs? Unfortunately, this scenario, known as restless legs syndrome (RLS), is more common than you think. In most cases, there are no direct causes of restless legs syndrome. And it can be very frustrating.
Restless legs syndrome is a pretty basic condition that affects up to 10% of adults in the U.S. However, the cause of restless legs syndrome is hard to determine. Conventional medicine treats RLS with harsh medications such as Requip, Mirapex, Horizant, and Neupro.1 These medications have harsh side effects such as stomach pain, constipation, nausea, vomiting or diarrhea. What’s more is that it doesn’t get to the root cause of your restless legs syndrome.
Not to worry! I’ll share some tried-and-true tips to find natural relief for restless legs syndrome to help you get optimal sleep. In order to find relief, you first need to know what could be the root cause of your restless legs syndrome.
What is Restless Legs Syndrome (RLS)?
Restless legs syndrome (RLS), also known as Willis-Ekbom disease, is essentially a sleep disorder.2 If you struggle to fall asleep because you have the strong urge to move their legs, you could have RLS. Restless legs syndrome can cause uncomfortable sensations in your legs such as a creeping, itchy, pulling, tugging, throbbing, burning and crawling feeling. Often, these sensations occur when you are lying down or after sitting for long periods.
People of any age can get restless legs syndrome, however the cause of restless legs syndrome differs from person to person. The chances of having restless legs syndrome increases significantly as you get older. You are also more at risk if you have a relative with restless legs syndrome. Let’s dive more into the symptoms of restless legs syndrome.
Symptoms of Restless Legs Syndrome
The defining symptom of restless legs syndrome is an overwhelming urge to move the legs, usually because of an uncomfortable sensation such as tingling, itching, throbbing, aching or feeling like electric shock. However, there are additional common symptoms that accompany restless legs syndrome. These include:
- Sensations that get worse after laying down or spending a long period of time sitting in a car, airplane, or a movie theater.
- You get temporary relief with movement such as stretching, jiggling your legs, or walking.
- Your symptoms are worse at night.
- Nighttime leg twitching.
Symptoms can go away for periods of time and then come back. In order to find relief, you have to get to the root cause of your symptoms. Let’s talk about restless legs syndrome causes.
6 Causes of Restless Legs Syndrome
In most cases, there is no direct cause of restless legs syndrome. However, genetics does play a significant role. If your symptoms develop before the age of 45, it is more likely that you have a first-degree relative such as a parent or sibling with RLS. While genetics plays a role in your risk of having restless legs syndrome, there is more evidence RLS could be caused by a hormone imbalance, autoimmune disease,3 nutrient deficiencies, and even pregnancy. Here are 6 common causes of restless legs syndrome:
Dopamine Imbalance
Dopamine is a neurotransmitter released by the substantia nigra, which is located below the thalamus of the brain. Your substantia nigra synthesises the amino acid tyrosine into a substance called dopa, which then turns into dopamine. This chemical messenger plays a role in several key body functions such as learning, motivation, heart rate, blood flow, sleep, mood, learning, and movement.
In a study conducted by Johns Hopkins Medicine, people with Parkinson’s disease, a condition that causes involuntary movements, had a significant decline in dopamine production and often developed restless legs syndrome. What’s more is that dopamine levels naturally decline towards the end of the day, which could explain why symptoms worsen in the evening.
Kidney Disease
Approximately 37 million people in the United States are living with kidney disease.4 Your kidneys are part of your body’s filter system. Their primary job is to remove waste and deliver nutrients to your blood. Your kidneys work in unison with your liver to remove waste. The kidneys’ filters remove excess salt and sugar from urine. Then, sodium-glucose contransposers reabsorb the filtered sugar and move it to the bloodstream. When these filters are forced to work hard they become permanently damaged and can eventually fail.
Diabetes and iron deficiency are associated with kidney disease, which I will discuss more in just a minute. Low iron is an effect of kidney disease and has shown to cause worsening symptoms of RLS.5 When kidney disease progresses, the ability to produce enough red blood cells is inhibited. As a result, less hemoglobin – an iron rich protein that acts as an oxygen taxi – production occurs, which further increases fatigue and muscle movement, also associated with RLS. Normal levels for hemoglobins are 13.5 to 17.5 gm/dL for men and 12.0 or 15.5 gm/dL for women.
Iron Deficiency
Iron is a mineral that the body needs for growth and development. Your body uses iron to make hemoglobin, a protein in red blood cells that carries oxygen from the lungs to all parts of the body, and myoglobin, a protein that provides oxygen to muscles. Your body also needs iron to make hormones such as cortisol, DHEA, and adrenaline.
As I just mentioned, kidney disease inhibits the body’s ability to produce red blood cells to carry oxygen in the bloodstream. This can lead to an iron deficiency, which can lead to dizziness or weakness, headache, pale or dry skin, a fast heart beat, or unintended movement in the lower leg.6
Many factors can cause an iron deficiency, such as a lack of vitamin B12 in your diet, or a B12 deficiency; blood disorders such as sickle cell disease; thyroid disease; or blood loss. Your doctor can test your iron levels with a standard blood test.
When checking for iron deficiency, be sure to ask your doctor to test your ferritin levels, rather than the standard iron tests, which measure your hemoglobin and hematocrit levels. Hemoglobin and hematocrit levels will only register as low if you have a severe iron deficiency, whereas ferritin is the storage protein for iron, and a better indication of the actual amount of iron available in your body. Your ferritin levels can be checked through a standard lab, and you should aim to keep your levels between 50-100 ng/mL.
Diabetes
Diabetes is a major health issue across the world. More than 32 million people in the United States have been diagnosed with diabetes or prediabetes, a condition where your blood sugar is higher than normal levels, yet not high enough to be diagnosed with type 2 diabetes.
Uncontrolled high blood sugars in people with diabetes can cause nerve damage, and may lead to diabetic peripheral neuropathy.7 Damage to the nerves of the feet and lower leg from peripheral neuropathy is a contributor to restless legs syndrome. Studies have shown that restless legs syndrome is more common in patients with type 2 diabetes than those with type 1 diabetes.
Rheumatoid Arthritis
Rheumatoid arthritis affects more than 1.3 million people in the United States. It is 2½ times more common in women than in men. It is an autoimmune disease that occurs when the body begins attacking the joints, mistaking them as foreign invaders.
Typically, rheumatoid arthritis starts in the small joints such as hands, fingers, and toes. Over time, it progresses to larger joints like the wrists, ankles, knees, and hips. The pain and swelling is usually on both sides of the body or in bi-lateral joints.
Pro-inflammatory proteins (called cytokines) that are produced by your immune system when you have rheumatoid arthritis impact sleep quality. Some small studies have shown elevated rates of restless legs syndrome in people with other autoimmune diseases, such as lupus.
Pregnancy
Pregnancy is another cause of restless legs syndrome, however it has more to do with lower levels of iron and folate than the pregnancy itself.8 As I mentioned, lower levels of iron can cause involuntary movement in the lower leg.
Hormonal changes during pregnancy, especially increases in the levels of estrogen and progesterone during the third trimester, are also likely a cause of restless legs syndrome. One study found that women had significant relief of restless legs syndrome symptoms 4 weeks after giving birth.9 Estrogen levels drastically fall after giving birth.
Diet
Caffeine and alcohol are the two main foods that trigger restless legs syndrome symptoms or make them worse. Caffeine is a natural stimulant found in coffee beans, tea leaves, and cocoa beans. It can also be produced synthetically like that found in soft drinks and most energy drinks. Caffeine promotes alertness by blocking the chemical messenger adenosine, a neurotransmitter that causes that sleepy feeling. Since restless legs syndrome is naturally a sleep disorder, logically, caffeine can make it even more difficult to go to sleep.
A common misconception is that alcohol helps you sleep. However, this couldn’t be further from the truth. It’s true that alcohol is a depressant that slows down your nervous system. It does allow you to fall asleep quickly, however drinking alcohol causes disruptions in the quality of your sleep. Several studies have shown an increase in restless legs syndrome symptoms after drinking alcohol.
Caffeine and alcohol are toxic foods, and should be avoided. If you must have them, it’s best to use them in moderation.
Testing for Restless Legs Syndrome
Because restless legs syndrome is caused by underlying conditions, there is not a lab test or scan that can be used to diagnose restless legs syndrome. However, your doctor can test for underlying medical conditions such as anemia, diabetes, or kidney disease that is linked to restless legs syndrome. Blood tests can measure your blood count, hemoglobin levels, basic organ functions, and thyroid hormone levels.
I found that the following ranges for hormone levels are where my patients at my clinic (and myself) thrived, not just lived:
- TSH levels of 1-2 UIU/ML or lower (Armour or compounded T3 can artificially suppress TSH)
- FT4 levels >1.1 NG/DL
- FT3 levels > 3.2 PG/ML
- RT3 levels < 10:1 ratio RT3:FT3
- TPO – TgAb levels < 4 IU/ML or negative
Remember, it is the individual level of each hormone that determines if your hormones are in balance. Conventional medicine tests for isolated hormones on their own, which will not pick up on whether your hormones are out of balance.
Labs such as Ulta Labs offer at-home tests for hemoglobin, liver and kidney function, and thyroid hormone levels.
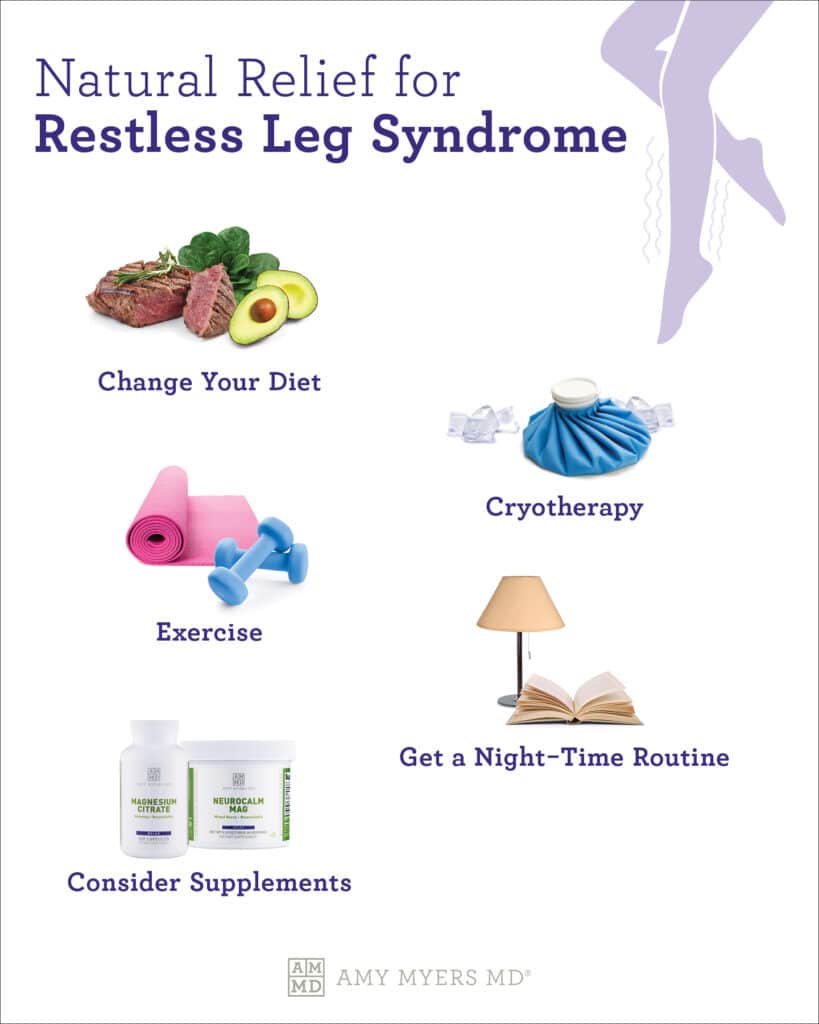
Natural Relief for Symptoms of Restless Legs Syndrome
Once you have discovered the root cause of restless legs syndrome, you can find relief from your symptoms without harsh medications or NSAIDs. Here’s a few steps you can take to get natural relief from restless legs syndrome.
 Dr. Amy Myers
September 19th, 2021
https://content.amymyersmd.com/article/causes-restless-legs-syndrome/Natural Relief for Restless Legs Syndrome – Infographic – Amy Myers MD®
Dr. Amy Myers
September 19th, 2021
https://content.amymyersmd.com/article/causes-restless-legs-syndrome/Natural Relief for Restless Legs Syndrome – Infographic – Amy Myers MD®Change Your Daily Diet
Vitamin and mineral deficiencies are common restless legs syndrome causes and linked to conditions such as diabetes and anemia, that contribute to restless legs syndrome symptoms.
Eating foods rich in protein are great sources of B vitamins and iron. Good sources of protein include grass-fed beef, free-range chicken, and wild-caught fish. I also recommend eating foods rich in electrolytes, including those high in magnesium, potassium, and calcium such as leafy green vegetables, avocados, sweet potatoes, and bananas.
Healthy fats help control blood glucose levels and can promote a healthy inflammatory response. Healthy fats include olive oil, avocado oil, and wild-caught seafood that are rich in omega-3 fatty acids.
In contrast, you should avoid toxic foods such as alcohol, caffeine, GMOs, artificial sweeteners, high-fructose corn syrup, processed foods, and sugar. These foods could make your restless legs syndrome symptoms worse.
Exercise
Remember, movement helps relieve restless legs syndrome symptoms. Regular exercise not only is essential for optimal health, it can also control your symptoms. I recommend 20-30 minutes of light to moderate exercise daily if you are experiencing restless legs syndrome symptoms. Make sure you pick an activity that keeps you moving such as taking a brisk walk. I enjoy doing yoga, hiking with my family, and swimming to get my body moving.
Cryotherapy
Have you heard about this “cool” new trend called cryotherapy? I bet you have! The word cryotherapy literally means “cold therapy.” It’s basically a term that can be used any time extreme cold is used as a form of treatment.
Inflammation is one of the first signs of autoimmune disease, which is a cause of restless legs syndrome. Several studies have confirmed that cryotherapy can reduce inflammation. Exposure to the extreme cold temperatures used for cryotherapy increases the presence of cytokine proteins IL-6, IL-1Ra, and IL-10. Cytokines, particularly the interleukins (abbreviated as “IL”), control cell signaling in an immune system response and support a healthy inflammatory response.
Establish a Bedtime Routine
Creating a bedtime routine is essential for several reasons, most notably better quality of sleep. Studies show that a regular sleep schedule promotes sound sleep quality. If you struggle to get to sleep, a bedtime routine can help turn off your brain and help you reach optimal sleep.
Try setting an alarm to wake you up in the morning, as well as for bedtime. You can use an app on your phone to manage a sleep schedule that will set an alarm to wake you up and silence your phone so you can get peaceful sleep. It’s important to go to bed and wake up at the same time every day, even on the weekend so your body is getting optimal rest.
Consider Supplements For Restless Legs Syndrome
In addition to these lifestyle changes, certain supplements can help reduce restless legs syndrome symptoms and address the root cause in the cases of vitamin and mineral deficiencies. Here are three supplements I recommend for those with restless legs syndrome:
The Myers Way® Multivitamin
The first supplement I always recommend everyone take is a high-quality multivitamin. The Myers Way® Multivitamin is designed for optimal absorption and bioavailability. I custom-formulated The Myers Way® Multivitamin to provide the widest range possible of the most critical vitamins and minerals in their most usable forms, which means methylated B vitamins, including 500 mcg of vitamin B12 and 400 mcg of folate to promote a healthy inflammatory response. My multivitamin does not have iron in it, so it’s important to eat enough iron rich foods such as grass-fed beef, free-range, organic chicken, and wild-caught salmon.
Complete Omega-3 Softgels
The benefits of omega-3 fatty acids are widely publicized. Omega-3 fatty acids support a healthy inflammatory response and may help lower the risk of chronic diseases like heart disease, cancer, and arthritis. And, because they are highly concentrated in the brain, omega-3 fatty acids are also important for memory, cognition, and behavior. My Complete Omega-3 softgels are pharmaceutical grade, GMP certified, and 3rd party tested by Eurofins. They are the purest, highest-potency fish oil supplement available on the market today.
Article Sources
- Restless Legs Syndrome Medications. Restless Legs Syndrome Foundation. 2021.
- Restless Legs Syndrome: An Overview. Cleveland Clinic. 2021.
- Restless Legs Syndrome. Autoimmune Registry. 2021.
- Kidney Disease / Chronic Kidney Disease. Cleveland Clinic. 2021.
- The Role of Iron in Restless Legs Syndrome. Richard P Allen and Christopher J Earley. Movement Disorders: Official Journal of the Movement Disorder Society, Vol. 22. 2007.
- Anemia: An Overview. Cleveland Clinic. 2021.
- Diabetic Neuropathy. The Global Diabetes Community. 2019.
- Pregnancy and RLS. WebMD. 2021.
- Elevated Estradiol Plasma Levels in Women with Restless Legs During Pregnancy. Andrea Dzaja, MD, et al. Elevated Estradiol Plasma Levels in Women with Restless Legs During Pregnancy. Sleep, Vol. 32. 2009.
